A Study on Functional Outcome of Comminuted Supracondylar Fracture Femur Treated by Plating with Fibular Bone Grafting
Sabarisree M1, Jyothiprasanth M2, Suresh Babu3 and Nithin Sunku4
DOI10.4172/2469-6684.100038
Sabarisree M1, Jyothiprasanth M2*, Babu S1 and Nithin Sunku3
1Department of Orthopaedic Surgery, Government Medical College, kottayam, Kerala, India
2Department of Orthopaedic Surgery, Government Taluk Hospital, Kuttyadi Calicut, Kerala, India
3Department of Orthopaedic Surgery, AKG Hospital, Kannur, Kerala, India
- *Corresponding Author:
- Jyothiprasanth M
Department of Orthopaedic Surgery
Government Taluk Hospital
Kuttyadi Calicut, Kerala, India
Tel: 9886389529
E-mail: jpmmnair@gmail.com
Received Date: February 02, 2017; Accepted Date: March 28, 2017; Published Date: April 04, 2017
Citation: Sabarisree M, Jyothiprasanth M, Babu S, et al. A Study on Functional Outcome of Comminuted Supracondylar Fracture Femur Treated by Plating with Fibular Bone Grafting. J Bone Rep Recomm. 2017, 3:1. doi: 10.4172/2469-6684.100038
Abstract
Introduction: Distal femur fractures are difficult, complex injuries that can result in devastating outcomes. The intra-articular injury can vary from a simple split to extensive comminution. Articular involvement can lead to posttraumatic arthritis. These fractures constitute 4% to 7% of all femur fractures. There is a bimodal distribution defined by the mechanism of injury. The goal of any treatment is to maintain or restore the congruity of the articular surface and restore the length and alignment of the femur and subsequently the limb.
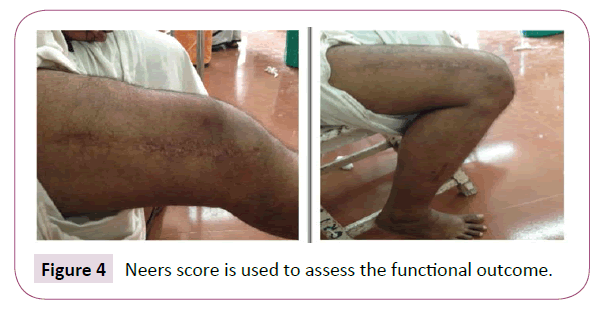
Materials and methods: A prospective study carried out from February 2015 to February 2016 in government medical college Thiruvananthapuram, involving 24 patients with comminuted supracondylar fracture femur (OTA/AO type A2, A3, C2 and C3) treated by distal femoral LCP with fibular bone grafting. The period of follow up was 12 months and the outcome was assessed using Neer’s score.
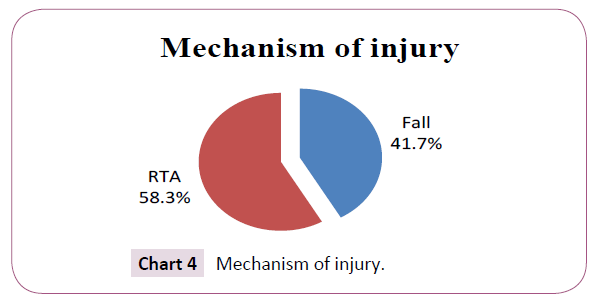
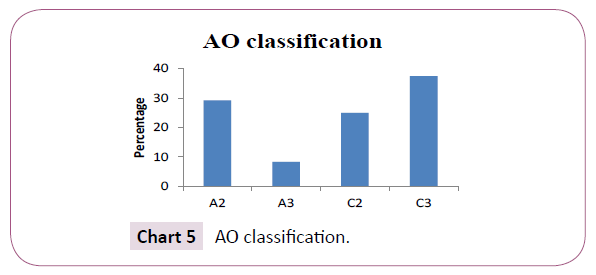
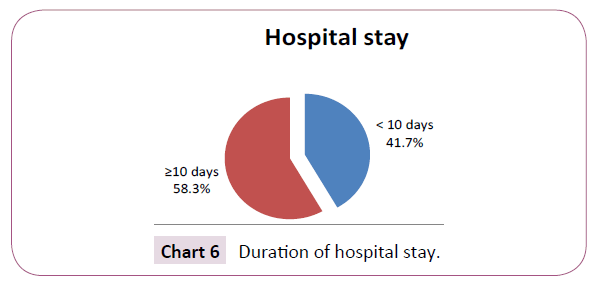
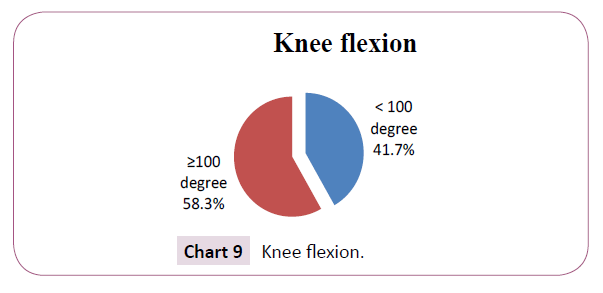
Results: 24 patients which included 16 males and 8 females with mean age of 45.7 showing a bimodal pattern in age distribution were studied. Mechanism of injury included both road traffic accident and fall in which 14 patients (58.3%) sustained the fracture due to RTA and 10 patients (41.7%) sustained injury due to fall affecting both sides equally. In the study according to AO/OTA classification there were 7 A2, 2 A3, 6 C2 and 9 C3 fractures. The average duration of hospital stay was 10 days with time delay to surgery of average 5 days and average duration of surgery 104 min. 14 patients (58.3%) had more than 100° of knee flexion and 10 patients (41.7%) had less than 100 degree. The minimum flexion obtained was 70° and maximum being 120°. There were 2 patients with varus angulation of 10 and 15° and shortening of 1 and 2 cm each. Complication included 1 case of non-union and 1 case of superficial wound infection which subsided with antibiotics. 3 cases with extensor lag with an average of 6°. Outcome assessment using Neer’s score showed 14 patients with excellent, 5 patients with good, 3 patients with fair and 2 patients with poor outcome.
Conclusion: Distal femoral LCP with fibular strut graft appears to be a good treatment option for comminuted supracondylar fracture of femur.
Keywords
Supracondylar; Femur; Distal femoral LCP; Fibular bone graft; Neer’s score
Introduction
Supracondylar area constitutes the distal 9-15 cm of distal femur. Fractures in this region are difficult, complex injuries that can result in devastating outcomes. These fractures are the result of severe axial load with virus, valgus or rotational force 1. These fractures of distal femur are very difficult to treat. It account for less than 7% of all femur fractures [1].
Supracondylar fractures of femur have a bimodal age distribution, with a high incidence in young adults from high energy trauma, such as motor vehicle accidents and a second peak in elderly with minor fall [2,3]. They are often unstable and comminuted and tend to occur in elderly or multiply injured patients following road traffic accidents 3. They may be associated with fractures of femoral neck, shaft, acetabulum, patella, tibia condyle and shaft. Associated ligament injury of knee has been reported in 20% cases [4]. Because of these reasons it is difficult to regain full knee motion and function. Poly trauma associated with the high velocity injuries makes the management extremely challenging. The incidence of malunion, non-union and infection are relatively high in many reported series3. It is one of the major challenges to an orthopaedic surgeon to treat this fracture with aim of achieving union and good range of motion at the knee.
Before development of techniques and implant to provide stable fixation, most distal femoral fractures were treated with skeletal traction. Studies done in 1960’s by Watson-Jones, Charley, and Neer et al. documented better outcome for patients treated non-operatively than for those treated operatively [5,6]. However, complications of non-operative treatment included angular deformity, joint incongruity, knee stiffness and delayed patient mobilization [7].
In 1970s, the AO (Arbeitsgemeinschaft fur Osteosynthesefragen) principles and the use of the angled blade plate revolutionized the treatment of these injuries [8-10]. Over the past years, the implants and techniques have improved. It is now recognized by most orthopaedic surgeons the distal femoral fractures are best treated by open reduction and internal fixation [11-24]. The goals in the treatment are the restoration of bone length, anatomic articular surface alignment and rotation, early mobilization of the associated joints rapid fracture union and minimal complications [25-28]. Although historically the results of operative techniques using internal fixation methods have presented with satisfactory results, the number of cases of non-union, loss of reduction and implant failure have been high [29-32].
Distal femoral LCP was developed by AO/ASIF in the late 1990s [33,34]. It is an implant system which can be used in the management of complex distal femoral fractures, primarily AO 33 A1-C3 fracture types [35]. It is a pre-contoured plate which approximates the anatomy of the lateral distal femur 33 and can be inserted through a minimally invasive lateral incision from distal to proximal into the endoperiosteal space after indirect, closed fracture reduction 36. The plate is then stabilized to the lateral aspect of the distal femur and proximally with locking screws through stab incisions [36]. The benefits of the distal femoral LCP over condylar buttress plates or dynamic condylar screws as reduced blood loss, lower infection rates and an ability to bridge the supracondylar fracture region as an internal fixator, without extensive dissection of bone fragment and associated periosteal stripping required for conventional plate fixation [37-44].
Bone grafting rates in the treatment of supracondylar femur fractures have been reported to range between 23% and 87% [45]. The use of a fibula to bridge the defects in long bones, especially in the management of bone tumours, has achieved variable success [46] to avoid common problems such as varus collapse and loss of fixation. The use of a fibular strut and corticocancellous graft helped to bridge the fragments with severe comminution, maintain limb length and counteract the relatively unstable distal femoral block from varus/valgus collapse. Immediate replantation and adequate fixation of the fibular graft to the proximal and distal ends of the bone to be grafted, along with placement of a cuff of cancellers bone at the host-graft junction and around the fibular strut, fostered early union of the graft to the host bone. The main disadvantage of this procedure may be the sequestration of the non-vascularised, autogenously fibular graft. Soft tissue preservation could also be important in achieving mechanical stability [47,48].
Materials and Methods
Functional outcome of comminuted supracondylar fracture femur treated by distal femoral LCP plating with fibular grafting
Study setting: Department of orthopaedics, Govt. Medical College, Thiruvananthapuram.
Study period: One year (February 2015-February 2016).
Study population: Patients with comminuted supracondylar fracture of femur admitted in department of Orthopaedics, Gov. Medical College and Thiruvananthapuram.
Period of follow-up: One year.
Statistical analysis: SPSS.
Data collection: Data collection is by clinical examination and interview method.
The study was a prospective study involving 24 patients with comminuted supracondylar fracture of femur from February 2015 to February 2016 treated by distal femoral LCP with fibular bone grafting.
All the cases were treated initially with emergency care as per ATLS principle in emergency room itself and then once the patient is stabilized, investigated pre-operatively. A case documentation form was used for data including age, gender, mechanism of injury, type of injury, side of injury and associated injuries.
All the study regarding my thesis was done at this institution only. All cases were operated at this institution only and being conducted by teachers and assisted by me. All data were collected by me and being showed and checked by my guide.
Inclusion criteria: Patients with age more than 18 sustaining comminuted supracondylar fracture femur.
Exclusion criteria:
• Pathological fracture
• Periprosthetic fracture
• Existing deformity to same limb
• Open fracture
• Polytrauma patients
Sample size:
Formula for calculating sample size 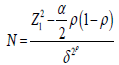
Where, p: Expected proportion; δ: Relative precision;  : Desired Confidence level=(95%).
: Desired Confidence level=(95%).
According to similar study “Treatment of Supracondylar Fracture of Distal Femur with Condylar Locking Compression Plating, Tapi Nalo 1, Amit Agrahari 2, Snehasish Datta 3, Vinil Paul 4, S. Nongthon Singh 5, Roel Langshong 6” Excellent functional outcome was 83.3%. Expected proportionrial dd=83.3%. Here, p=83.3%; δ: Relative precision (20% of p); 1-a/2: Desired Confidence level=(95%); N=19. In our study, we got the follow up of 24 patients.
Management of patient: On arrival of the patient in the emergency room, initial emergency management is carried out by maintaining airway, breathing and circulation. Thorough assessment of the patient is then done to rule out head, chest, spinal or pelvic injury. Musculoskeletal examination is done to look for associated fractures. Stabilization of the patient with intravenous fluids, oxygen and blood transfusion as required. The distal neurovascular status is carefully assessed. Then the fractured extremity is immobilised in a Thomas splint and sent for radiological examination. For open fractures thorough irrigation and lavage, debridement, intravenous antibiotics and delayed wound closure is done. Lower tibia skeletal traction is applied using a Steinmann pin or Denham pin under local anaesthesia followed by continuous traction is given using Buhler Braun splint in ward.
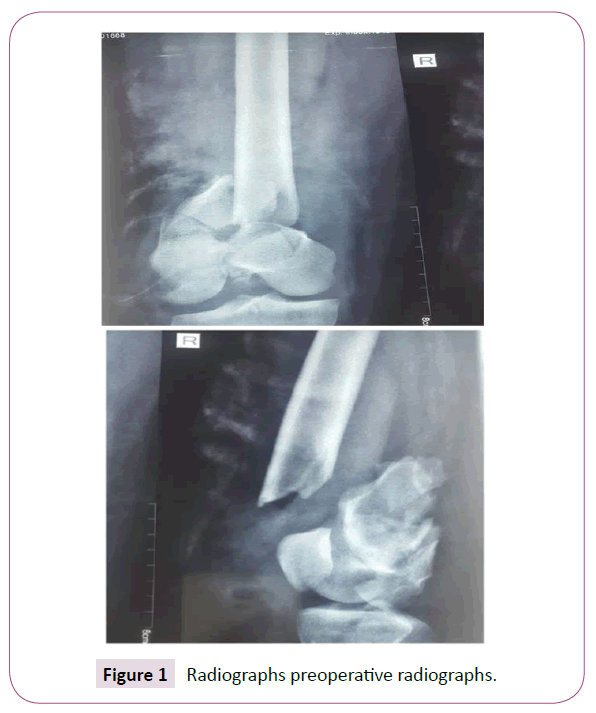
Pre-operative assessment: On admission relevant investigations for surgical workup are done in all patients which include hemogram, blood sugar level, renal function test, liver function test, blood grouping, Rh typing, bleeding time, clotting time, retroviral screening, hepatitis B antigen assay, hepatitis C antigen assay. Medical disorders are optimized before surgery (Figure 1).
Fracture is classified according to the AO classification with the help of radiographs. Preoperative planning is done to assess the size of plate and screws to be used.
The limb to be operated is prepared. Third generation cephalosporin given early morning on the day of surgery.
Surgical procedure: Anaesthesia-spinal, epidural or general anaesthesia.
Patient positioned supine on the operating table with a pillow below the knee to flex the knee. A pneumatic tourniquet is applied in the upper thigh. Tibia pin id then removed, the limb is scrubbed with povidone iodine. Ipsilateral iliac crest and contralateral leg is also prepared.
Lateral standard approach is mostly used. A lateral incision parallel to the shaft of femur, extending across the midpoint of lateral femoral condyle, anterior to fibular collateral ligament, across the knee and gently curved anteriorly to end distal and lateral to tibial tubercle. The vastuslateralis is elevated from the lateral intermuscular septum and retracted anteriorly and medially exposing the distal femur (Figure 2).
The condyles are reduced and stabilised temporarily by k wires and fixed with cancellous screws. Fibular strut graft is harvested from the ipsilateral side and inserted in the medullary cavity of the proximal femur and into the distal femur maintaining axial and coronal alignment. Supracondylar part is reduced and distal femoral LCP placed. Cancellous bone graft from the iliac crest is placed to fill the gap. Wound is closed in layers after attaining haemostasis over suction drain.
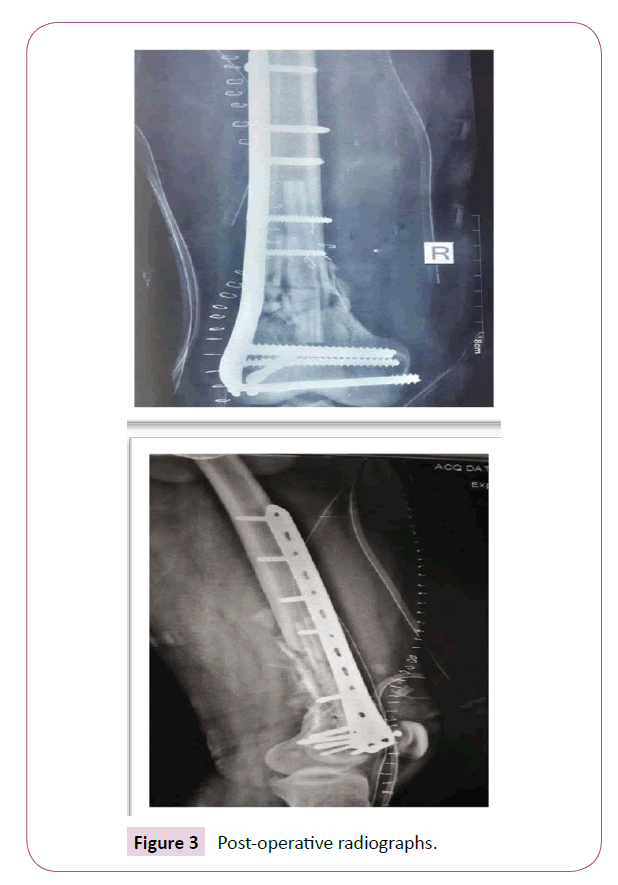
Postoperative period: Vitals of the patients are monitored. Blood transfusion was given if postoperative haemoglobin is below 9 g/dl. Intravenous antibiotics are continued in the postoperative period for 5 days and oral antibiotics till suture removal. Analgesics are given as per patient’s compliance. Sutures removal done on the 14th postoperative day (Figures 3 and 4).
Discharge: Patients are discharged once the surgical wound is healed and the general condition is stable.
Follow up: All patients are followed up at 2 weeks, 6 weeks, 2 months, 3 months, 6 months and 1 year. At every visit patient is assessed both clinically and using radiographs (Table 1).
| Functional [70 points] | |
|---|---|
| A) Pain [20 points] | |
| No pain | 20 |
| intermittent | 16 |
| with fatigue | 12 |
| limits function | 8 |
| constant or at excretion | 4 |
| B) Walking capacity [20 points] | |
| Same as before accident | 20 |
| Mild restriction | 16 |
| Restriction stair sideways | 12 |
| Severe/cane | 8 |
| Crutches/brace | 4 |
| C) Movements-Flexion |20 points) | |
| Normal or 135 | 20 |
| Upto 100° | 16 |
| Upto 80° | 12 |
| Upto 60" | 8 |
| Upto 40° | 4 |
| Upto 20° | 0 |
| D) Work capacity [10 points] | |
| As before | 10 |
| Regular with handicap | 8 |
| Alter work | 6 |
| Light work | |
| No work | 2 |
Table 1: Neer’s criteria.
Results and Analysis
In our study, incidence of fracture is (Table 2) high in young patients and elderly (Chart 1).
| Age in years | Frequency | Percent |
|---|---|---|
| 20-29 | 8 | 33.3 |
| 30-39 | 4 | 16.7 |
| 40-49 | 2 | 8.3 |
| 50-59 | 4 | 16.7 |
| More than 60 | 6 | 25 |
Table 2: Age distribution.
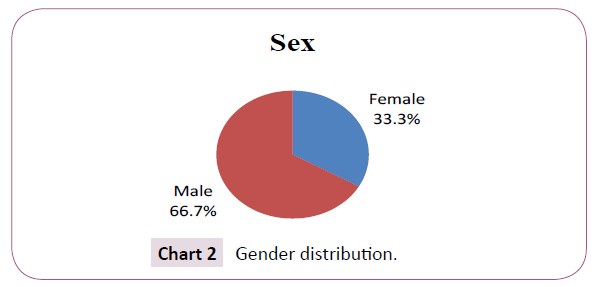
In the study of 24 patients, 16 (66.7%) are (Table 3) males and 8(33.3%) are females (Chart 2).
| Sex | Frequency | Percent |
|---|---|---|
| Female | 8 | 33.3 |
| Male | 16 | 66.7 |
| Total | 24 | 100.0 |
Table 3: Gender distribution.
In the study, both (Table 4) sides affected equally (Chart 3).
| Side | Frequency | Percent |
|---|---|---|
| Left | 12 | 50.0 |
| Right | 12 | 50.0 |
| Total | 24 | 100.0 |
Table 4: Side distribution.
In the study, 14(58.3%) patients sustained fracture due (Table 5) to RTA and 10(41.7%) patients by fall. Of this RTA majority were below the age of 30 and among those fall majority were elderly (Chart 4).
| Mechanism of injury | Frequency | Percent |
|---|---|---|
| Fall | 10 | 41.7 |
| RTA | 14 | 58.3 |
| Total | 24 | 100.0 |
Table 5: Mechanism of injury.
In our study among comminuted (Table 6) supracondylar fracture 9(37.5%) were extra-articular fractures and 15 (72.5%) were intra-articular (Chart 5).
| AO classification | Frequency | Percent |
|---|---|---|
| A2 | 7 | 29.2 |
| A3 | 2 | 8.3 |
| C2 | 6 | 25.0 |
| C3 | 9 | 37.5 |
| Total | 24 | 100.0 |
Table 6: AO classification.
The average duration of (Table 7) hospital stay is 10 days (Chart 6).
| Hospital stay | Frequency | Percent |
|---|---|---|
| <10 days | 10 | 41.7 |
| ≥10 days | 14 | 58.3 |
| Total | 24 | 100.0 |
Table 7: Duration of hospital stay.
The average time delay between (Table 8) admission and surgery is 5 days (Chart 7).
| Time delay | Frequency | Percent |
|---|---|---|
| <7 days | 19 | 79.2 |
| ≥7 days | 5 | 20.8 |
| Total | 24 | 100.0 |
Table 8: Time delay to surgery.
The average duration (Table 9) of surgery is 104 min (Chart 8).
| Duration of Surgery | Frequency | Percent |
|---|---|---|
| <100 min | 5 | 20.8 |
| ≥100 min | 19 | 79.2 |
| Total | 24 | 100.0 |
Table 9: Duration of surgery.
14 patients (58.3%) had more than 100° (Table 10) of knee flexion and 10 patients (41.7%) had less than 100 degree. The minimum flexion obtained was 70° and maximum being 120° (Chart 9).
| Knee flexion | Frequency | Percent |
|---|---|---|
| <100° | 10 | 41.7 |
| ≥100° | 14 | 58.3 |
| Total | 24 | 100.0 |
Table 10: Knee flexion.
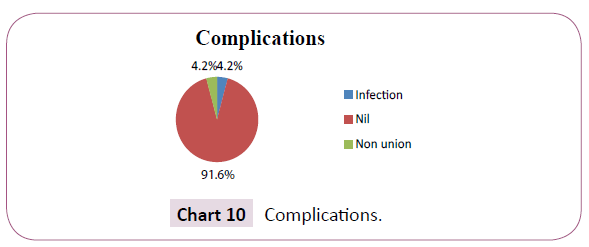
There was one case of non-union and one case of superficial (Table 11) wound infection which subsided by intravenous antibiotic treatment (Chart 10).
| complication | Frequency | Percent |
|---|---|---|
| Infection | 1 | 4.2 |
| Non union | 1 | 4.2 |
| Nil | 22 | 91.7 |
| Total | 24 | 100.0 |
Table 11: Complications.
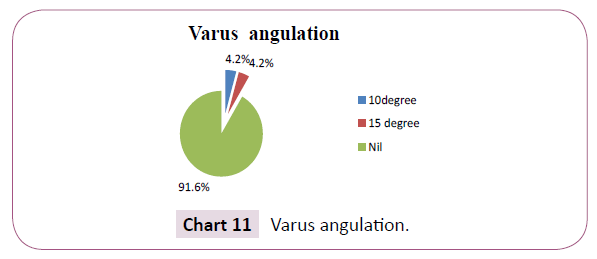
In the study 2 patient had varus angulation among them one had 10° of angulation and other had 15° of angulation (Chart 11).
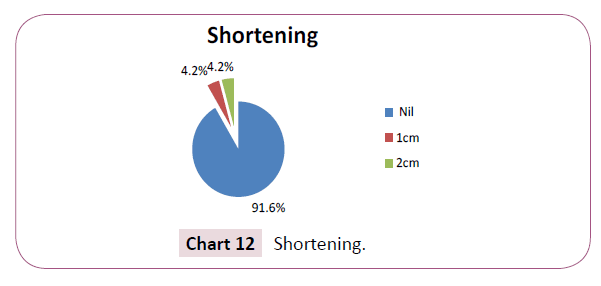
In the study 2 patients had shortening among (Tables 12 and 13) them one had 1 cm shortening and the other had 2 cm shortening (Chart 12)?
| Varus angulation | Frequency | Percent |
|---|---|---|
| 10° | 1 | 4.2 |
| 15° | 1 | 4.2 |
| Nil | 22 | 91.7 |
| Total | 24 | 100.0 |
Table 12: Varus angulation.
| Shortening | Frequency | Percent |
|---|---|---|
| Nil | 22 | 91.6 |
| 1 cm | 1 | 4.2 |
| 2 cm | 1 | 4.2 |
| Total | 24 | 100.0 |
Table 13: Shortening.
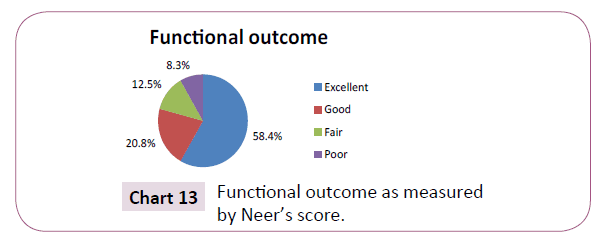
In the study 14(58.4%) had excellent functional (Table 14) outcome, 5(20.8%) had good functional outcome, 3(12.5%) had fair functional outcome and 2 patients (8.35%) had poor outcome (Chart 13).
| Functional outcome | Frequency | Percent |
|---|---|---|
| Excellent | 14 | 58.3 |
| Good | 5 | 20.8 |
| Fair | 3 | 12.5 |
| Poor | 2 | 8.3 |
| Total | 24 | 100.0 |
Table 14: Functional outcome as measured by Neers score.
The functional outcome of 11(91.7%) patients out of 12 patients with age less than 40 years is excellent to good and only 1(8.3%) patient had unsatisfactory to poor outcome, similarly out of 12 patients with age more than 40 years 8(66.7%) patients had excellent or good outcome and 4(33.3%) had unsatisfactory or poor outcome (Table 15).
| Functional outcome | Total | ||
|---|---|---|---|
| Age | Excellent- good | Unsatisfactory-poor | |
| Less than 40 years | 11 | 1 | 12 |
| more than or equal to 40 years | 8 | 4 | 12 |
| Total | 19 | 5 | 24 |
Odds ratio-5.5 and p value-0.317
Table 15: Comparison of age and functional outcome.
Out of 14 patients who sustained fracture due to RTA, 12(85.7%) had excellent or functional outcome and 2(14.3%) had unsatisfactory or poor outcome while out of 10 patients sustained injury due to fall 7(70%) had excellent to good functional outcome and 3(30%) had unsatisfactory to poor outcome (Table 16).
| Mechanism of injury | functional outcome | Total | |
|---|---|---|---|
| Excellent- good | Unsatisfactory- poor | ||
| RTA | 12 | 2 | 14 |
| Fall | 7 | 3 | 10 |
| Total | 19 | 5 | 24 |
Odds ratio-2.5 and p value-0.615
Table 16: Comparison of mechanism of injury and functional outcome.
Out of 16 males who were treated 14(87.5%) had excellent to good outcome and 2(12.5%) had unsatisfactory to poor outcome and out of 8 females who underwent surgery 5(62.5%) had excellent to good outcome and 3(37.5%) had unsatisfactory to poor outcome (Table 17).
| Functional outcome | Total | ||
|---|---|---|---|
| Sex | Excellent- good | Unsatisfactory-poor | |
| Male | 14 | 2 | 16 |
| Female | 5 | 3 | 8 |
| Total | 19 | 5 | 24 |
Odds ratio-4.2 p value-0.289
Table 17: Comparison of sex and functional outcome.
Out of 9 extra-articular fractures, 7 (77.8%) had excellent to good outcome and 2 (22.2%) had unsatisfactory to poor outcome and out of 15 intra-articular fractures 12 (80%) had excellent to good outcome and 3 (20%) had unsatisfactory to poor outcome (Table 18).
| Functional outcome | Total | ||
|---|---|---|---|
| Type of fractures | Excellent- good | Unsatisfactory-poor | |
| Extra-articular fractures | 7 | 2 | 9 |
| Intra-articular fractures | 12 | 3 | 15 |
| Total | 19 | 5 | 24 |
p value-0.897
Table 18: Comparison of type of fracture and functional outcome.
In patients with age less than 40 years, 10 patients sustained fracture due to RTA and 2 patients sustained injury due to fall and in patients with age more than 40 years only 5 patients sustained fracture due to RTA and 7 patients sustained fracture due to fall (Table 19).
| Mechanism of injury | Total | ||
|---|---|---|---|
| Age | RTA | Fall | |
| Less than 40 | 10 | 2 | 14 |
| More than 40 | 5 | 7 | 12 |
| Total | 15 | 9 | 24 |
Table 19: Comparison of age and mechanism of injury.
Among (Table 20) males 12 patients sustained injury due to RTA and 4 patients sustained injury due to fall, among females 2 patients sustained injury due to RTA and 6 patients sustained injury due to fall.
| Mechanism of injury | Total | ||
|---|---|---|---|
| Sex | RTA | fall | |
| Men | 12 | 4 | 16 |
| Female | 2 | 6 | 8 |
| Total | 14 | 10 | 24 |
Table 20: Comparison of sex and mechanism of injury.
Extension lag: In our study there were 3 cases with extensor lag the average being 6°.
Fracture union: Fracture union is defined as the ability of the patient to fully weight-bear without discomfort in the presence of radiological bridging callus on three cortices, assessed on standard AP and lateral radiographs. The time taken for union in our study ranges from 14 weeks to 19 weeks with a mean of 13.5 weeks.
Discussion
Comminuted supracondylar fractures of femur historically have been difficult to treat. Problems such as varus collapse, malunion and noun ion frequently resulted before fixed angle plates and indirect reduction techniques were popularized. In our study an attempt is made to assess the functional outcome of comminuted supracondylar fracture of femur treated distal femoral locking plate with fibular bone grafting. The study was conducted on 24 patients with comminuted supracondylar fracture admitted in department of Orthopaedics, Gov. Medical College and Thiruvananthapuram.
Age distribution
In our study age distribution show a bimodal pattern, 8 patients (33.3%) with age less than 30 years and 6 patients (25%) with age more than 60 sustained the fracture and 10 patients (41.7%) sustained fracture in the intermediate group.
In the study by Schatzker et al. [2] also showed a bimodal distribution with 25% of patients in the second and third decade and more than 60% of patients above 60 years.
Average age group in other studies
1. Tapi nalo et al. 59–The maximum age of the patient in the present study was 70 years and minimum being 18 years, with mean age of 27.50 years.
2. EJ Yeap et al. 60–The patient’s ages ranged from 15 to 85 with a mean of 44.
3. Srinath et al. 61–The median age was 47 years ranging from 28-70 years.
4. Wong et al. 62–The mean age was 75 years with a range from 62 -101 years.
5. Schütz et al. 63–The mean age is 52 years.
Bimodal distribution is due to high incidence of this fracture in young adults due to high energy injury and secondary peak in elderly osteoporotic people.
Gender distribution
In the study of 24 patients, 16 (66.7%) are males and 8(33.3%) are females. In comparison with other studies:
1. Tapi nalo et al. 59–out of 30 patients, 23 were males and 7 were females
2. Srinath et al. 61–out of 20 patients, 13 patients were females and 7 patients were females
3. Wong et al. 62–among 16 patients, there was only 1 male and 15 were females.
Side distribution
In the study, both sides affected equally. Other studies:
1. EJ Yeap et al. 60–Seven fractures involved the right side and four involved the left.
2. Srinath et al. 61–12 patients were with fracture on right side and 8 on left side.
Mechanism of injury
In the study, 14 (58.3%) patients sustained fracture due to RTA and 10 (41.7%) patients by fall. Of this RTA majority were below the age of 30 and among those fall majority were elderly.
As compared to other studies
1. EJ Yeap et al. 60–The causes of fractures was motor vehicle accident in seven patients and a fall in four patients. There were no sports or industrial accidents. One patient sustained multiple fractures including lung injury which required ventilation.
2. Srinath et al. 61–15 of the fractures was caused by road traffic accidents and 3 were due to fall, 2 were due to assault.
3. Wong et al. 62–majority of patients had low-energy trauma with 15 patients having falls on level ground. One patient was knocked down by a vehicle in a road traffic accident and 13 patients had isolated injuries while three had multiple fractures.
4. Weight et al. 64–26 patients with 27 high-energy fractures of the distal femur. Mechanism of injury included 12 motor vehicle collisions, 4 high falls, 5 motorcycle crashes, and 1 bicyclist struck by a car.
Preoperative radiological classification
In our study among comminuted supracondylar fracture 9(37.5%) were extra-articular fractures and 15(72.5%) were intra-articular: AO/OTA types.
Extra articular fractures
A2-7 cases and A3-2 cases.
Intra articular fractures
C2-6 cases and C3-9 cases.
Other studies:
1. Yeap et al. 60–According to the AO classification system, there were four Type A1, two Type A3, one Type C1, one Type C2 and three Type C3 fractures.
2. Srinath et al. 61–Of the 20 fractures two were type A1, two were type A2, three were type C1, nine were type C2 and four were type C3.
3. Wong et al. 62–eight patients had type A, three type B and five type C fractures.
4. Weight et al. 64–There was 4 A2, 3 A3, 12 C2, and 3 C3 fractures.
5. Apostolou 65–One type 41A, two type 41B, six type 41C, four type 33A and four type 33C.
Hospital stay
In our study the average duration of hospital stay is 10 days.
Comparing with other studies:
1. Nalo et al. 59–The mean duration of hospitalisation for all patients was 18.77 days (range, 14-29 days).
2. Yeap et al. 60–The average length of hospitalisation was 17.2 days with a range of 8 to 34 days.
Time delay
In our study, the average time delay between admission and surgery is 5 days when compared with other studies:
1. Nalo et al. 59–The mean time to operation for closed fracture was 8.96 ± 3.2 days (7-14) days and mean time to operation for open fracture was 11.20 ± 3.88 days (7-14) days.
2. Yeap et al. 60–The average number of days from injury to surgery was 9.9 days with a range of 4 to 19 days.
3. Srinath et al. 61–All the surgeries were done within 3 days after admission.
4. Wong et al. 62–All patients were treated surgically within one week of the injury.
Duration of surgery
In our study the average duration of surgery is 104 min, as compared to other studies:
1. EJ Yeap et al. 60–The operative time ranged from 80 to 180 min, with an average of 119.2 min.
2. Srinath et al. 61–Average time duration of surgery was 101 min with shortest duration being 80 min and longest being 130 min. Type C3 fractures accounting for longest surgical time.
3. Schütz et al. 63–The mean duration of surgery was 85 min (range 40-135 min) for 33A fractures and 149 min (range 50-300 min) for 33C fractures.
Knee flexion
In our study, 14 patients (58.3%) had more than 100° of knee flexion and 10 patients (41.7%) had less than 100 degree. The minimum flexion obtained was 70° and maximum being 120°. On comparison:
1. EJ Yeap et al. 60–Mean extension was 1° (range 0° to 5°), with mean flexion 107.7° (range 40° to 140°). Mean range of motion was from 1° to 107.7°.
2. Srinath et al. 61–Average knee flexion was from neutral to 104° with more than 60% patients having knee range of motion from neutral to 110 degree.
3. Wong et al. 62–Concerning the range of motion, six patients had full, nine had slightly limited and one had severely limited range of knee motion.
4. Schütz et al. 63–After fracture healing, maximum flexion of the injured limb was on average 80% of the range of the uninjured limb.
5. Weight et al. 64–The average knee range of motion was 5° to 114°.
Fracture union
The time taken for union in our study ranges from 14 weeks to 19 weeks with a mean of 13.5 weeks.
1. Tapi Nalo et al. 59–Clinical union was seen at a mean time of 14.47 weeks (range, 9-32 weeks). Radiologically, bridging callus was seen at 12-16 post-operative weeks and the mean time to complete radiological union was 26.47 weeks (range, 20-40 weeks).
2. EJ Yeap et al. 60–Average time to union was 18 weeks with a range from 6 weeks to 36 weeks.
3. Srinath, et al. 61–Of 20 patients, 14 Patients (70%) showed radiological union within 18 weeks. Remaining united by 28 weeks. None had implant failure or non-union.
4. Wong et al. 62–Union was defined radio graphically as presence of bony trabecular across the fracture site. All fractures united with an average union time of 30 (16-68) weeks.
5. Weight et al. 64–All fractures healed without secondary surgeries at a mean of 13 weeks (range 7-16 weeks).
6. Apostolou et al. 65–Bony union was achieved on average in 12.5 weeks.
7. Ramesh et al. 66–Union was achieved in all cases by an average time of 19 weeks.
Complications
There was one case of non-union and one case of superficial wound infection in our study which subsided by intravenous antibiotic treatment.
Complications in similar studies
1. Tapi Nalo et al. 59–There were no intra-operative and immediate post-operative complications. Two case of superficial infection was managed by antibiotics and local wound dressing.
2. Yeap et al. 60–Complications included one implant fracture which required revision to another DF-LCP. There was one mal-alignment of the lower limb. One plate was cutting out due to poor fixation. There were no non-unions, deep infections or removal of implants due to ilia-tibial tract pain.
3. Srinath et al. 61–2 patients had signs of early postoperative infection which settled with redebridement and intravenous antibiotics.
4. Wong et al. 62–There was no infection. However, there were two cases with failure of fixation, which occurred early in our series. Both were loosening of the proximal fixation of LISS.
5. Weight et al. 64–There were no cases of failed fixation, implant breakage, or infection.1 mal-union where the fracture was fixed in 8° of valgus and 2 cases of external rotation between 10° and 15°. Painful hardware occurred in 4 patients.
6. Schütz et al. 63–deep infection requiring several debridement’s occurred in 2 patients.
Varus angulation and shortening
In the study 2 patient had varus angulation among them one had 10° of angulation and other had 15° of angulation and 2 patients had shortening among them one had 1 cm shortening and the other had 2 cm shortening. In similar studies:
1. Yeap et al. 60–There was varus angulation of 10°, internal rotation of 5°, and limb length discrepancy of 2 centimetres.
2. Srinath et al. 61–Out of 20 patients nine had shortening; 8 patients with shortening of 2 cm and 1 patient with shortening of 3 cm. Patient with 3 cm shortening was managed with heel raise. One patient had 15° varus misalignment, which was in our initial part of study.
3. Schütz et al. 63–Assessment of valgus/varus alignment showed a deviation of 5-10° in 13 cases, and a 10-20° deviation in 1 case.
4. Weight et al. 64–A comparison of postoperative to healed final radiographs for each femur demonstrated no case with greater than a 3° difference in either varus or valgus.
Extensor deficit
In our study there were 3 cases with extensor lag the average being 6°.
Srinath et al. 61–Average knee extensor lag was 5°.
Schütz et al. 63–An extension deficit of more than 5° was measured in 3 cases.
Functional outcome
In the study 14(58.4%) had excellent functional outcome, 5(20.8%) had good functional outcome, 3(12.5%) had fair functional outcome and 2 patients (8.35%) had poor outcome, as compared to:
1. Tapi Nalo et al. 59–Based on Neer’s scoring system the final outcome for all cases was Excellent in 25 (83.33%), good in 3 (13.33%) and fair in 1 (3.33%) patients.
2. Yeap et al. 60–Using the Schatzker scoring system, there were four excellent results, four good, two fair and one failure.
3. Srinath et al. 61–According to NEER’S Score 13 patients (65%) showed excellent result. 3 Patients (15%) showed good outcome, 4 patient (20%) showed fair outcome and none showed poor outcome.
Comparison of age and functional outcome
The functional outcome of 11(91.7%) patients out of 12 patients with age less than 40 years is excellent to good and only 1(8.3%) patient had unsatisfactory to poor outcome, similarly out of 12 patients with age more than 40 years 8(66.7%) patients had excellent or good outcome and 4(33.3%) had unsatisfactory or poor outcome.
Comparison of mechanism of injury and functional outcome
Out of 14 patients who sustained fracture due to RTA, 12(85.7%) had excellent or functional outcome and 2(14.3%) had unsatisfactory or poor outcome while out of 10 patients sustained injury due to fall 7(70%) had excellent to good functional outcome and 3(30%) had unsatisfactory to poor outcome.
Comparison of sex and functional outcome
Out of 16 males who were treated 14(87.5%) had excellent to good outcome and 2(12.5%) had unsatisfactory to poor outcome and out of 8 females who underwent surgery 5(62.5%) had excellent to good outcome and 3(37.5%) had unsatisfactory to poor outcome.
Comparison of type of fracture and functional outcome
Out of 9 extra-articular fractures, 7 (77.8%) had excellent to good outcome and 2 (22.2%) had unsatisfactory to poor outcome and out of 15 intra-articular fractures 12 (80%) had excellent to good outcome and 3 (20%) had unsatisfactory to poor outcome.
Comparison of age and mechanism of injury
In patients with age less than 40 years, 10 patients sustained fracture due to RTA and 2 patients sustained injury due to fall and in patients with age more than 40 years only 5 patients sustained fracture due to RTA and 7 patients sustained fracture due to fall.
Comparison of sex and mechanism of injury
Among males 12 patients sustained injury due to RTA and 4 patients sustained injury due to fall, among females 2 patients sustained injury due to RTA and 6 patients sustained injury due to fall [49-62].
Conclusion
In our study age distribution show a bimodal pattern, 8 patients (33.3%) with age less than 30 years and 6 patients (25%) with age more than 60 sustained the fracture and 10 patients (41.7%) sustained fracture in the intermediate group.
In our study the mechanism of injury included road traffic accident and fall. 14 patients (58.3%) sustained the fracture due to RTA and 10 patients (41.7%) sustained injury due to fall.
In our study 16 (66.7%) are males and 8(33.3%) are females, Among males 12 patients (75%) sustained injury due to RTA and 4 (25%) patients sustained injury due to fall, among females 2 patients (25%) sustained injury due to RTA and 6 patients (75%) sustained injury due to fall
In our study among comminuted supracondylar fracture 9(37.5%) were extra-articular fractures and 15(72.5%) were intra-articular.
14 patients (58.3%) had more than 100° of knee flexion and 10 patients (41.7%) had less than 100°. The minimum flexion obtained was 70° and maximum being 120°. Average being 100°.
The average duration of hospital stay is 10 days. The average time delay between admission and surgery is 5 days. The average duration of surgery is 104 min.
Excellent to good functional outcome as assessed by Neer’s score is obtained in 19 patients (79.1%) and fair to poor outcome was obtained in 5 patients (20.8%).
The functional outcome of 11(91.7%) patients out of 12 patients with age less than 40 years is excellent to good and only 1(8.3%) patient had unsatisfactory to poor outcome, similarly out of 12 patients with age more than 40 years 8(66.7%) patients had excellent or good outcome and 4(33.3%) had unsatisfactory or poor outcome.
Out of 16 males who were treated 14(87.5%) had excellent to good outcome and 2(12.5%) had unsatisfactory to poor outcome and out of 8 females who underwent surgery 5(62.5%) had excellent to good outcome and 3(37.5%) had unsatisfactory to poor outcome.
Out of 9 extra-articular fractures, 7 (77.8%) had excellent to good outcome and 2 (22.2%) had unsatisfactory to poor outcome and out of 15 intra-articular fractures 12 (80%) had excellent to good outcome and 3 (20%) had unsatisfactory to poor outcome.
There was one case of non-union and one case of superficial wound infection which subsided by intravenous antibiotic treatment.
In the study 2 patient had varus angulation among them one had 10° of angulation and other had 15° of angulation.
In the study 2 patients had shortening among them one had 1 cm shortening and the other had 2 cm shortening?
In the study there were 3 cases with extensor lag with average being 6°.
Distal femoral LCP is a good implant in fixation of comminuted supracondylar fracture of femur. When augmented with fibular strut grafting it prevented varus collapse in majority of cases in the study population.
References
- Court-Brown CM, Heckman JD, McQueen MM, Ricci WM, Tornetta P (2014) editors Rockwood & Green's Fractures in Adults.
- Schatzker J, Home G, Waddell J (1974) The Toronto experience with the supracondylar fracture of the femur 1966-1972. Injury 6: 113-123.
- Terry Canale S, James H (1980) Beaty editors Campbell's Operative Orthopaedics.
- Walling AK, Seradge H, Speigel PG (1982) Injuries to the knee ligaments with fractures of the femur. J Bone Joint Surg Am 64: 1324-1327.
- Neer CS, Grantham SA, Shelton ML (1967) Supracondylar fracture of the adult femur. J Bone Joint Surg Am 49: 591-613.
- Stewart MJ, Sisk TD, Wallace SL (1966) Fractures of the distal third of the femur. J Bone Joint Surg Am 48: 784-807.
- Healy WL, Brooker AF (1983) Distal femoral fractures: comparison of open and closed methods oftreatment. Clin Orthop Relat Res 174: 166-171.
- Chiron HS, Tremoulet J, Casey P (1974) Fractures of the distal third of the femur treated by internal fixation. Clin Orthop Relat Res 100: 160-170.
- Olerud S (1972) Operative treatment of supracondylar-condylar fractures of the femur: technique and results in fifteen cases. J Bone Joint Surg Am 54: 1015-1032.
- Schatzker J, Lambert DC (1979) Supracondylar fractures of the femur. Clin Orthop Relat Res 136: 77-83.
- Giles JB, Delee JC, Heckman JD (1982) Supracondylar-intercondylar fractures of the femur treated with a supracondylar plate and lag screw. J Bone Joint Surg Am 64: 864-870.
- Hall MF (1978) Two-plane fixation of acute supracondylar and intracondylar fractures of the femur. South Med J 71: 1474-1481.
- Halpenny J, Rorabeck CH (1984) Supracondylar fractures of the femur: results of treatment in 61 patients. Can J Surg 27: 606-609.
- Iannacone WM, Bennett FS, Delong WG (1994) Initial experience with the treatment of supracondylar femoral fractures using the supracondylar intramedullary nail: a preliminary report. J Orthop Trauma 8: 322-327.
- Leung KS, Shen WY, Mui LT (1991) Interlocking intramedullary nailing for supracondylar and intercondylar fractures of the distal part of the femur. J Bone Joint Surg Am 73: 332-340.
- Lucas SE, Seligson D, Henry SL (1993) Intramedullary supracondylar nailing of femoral fractures: a preliminary report of the GSH supracondylar nail. ClinOrthopRelat Res 296: 200-206.
- Marks DS, Isbister ES, Porter KM (1994) Zickel supracondylar nailing for supracondylar femoral fractures in elderly or infirm patients: a review of 33 cases. J Bone Joint Surg Br 76: 596-601.
- Mize RD, Bucholz RW, Grogan DP (1982) Surgical treatment of displaced, comminuted fractures of the distal end of the femur. J Bone Joint Surg Am 64: 871-879.
- Radford J, Howell CJ (1992) The AO dynamic condylar screw for fractures of the femur. Injury 23: 89-93.
- Sanders R, Regazzoni P, Ruedi TP (1989) Treatment of supracondylar-intracondylar fractures of the femur using the dynamic condylar screw. J Orthop Trauma 3: 214-222.
- Sanders R, Swintkowski M, Rosen H (1991) Double-plating of comminuted, unstable fractures of the distal part of the femur. J Bone Joint Surg Am 73: 341-346.
- Schatzker J (1998) Fractures of the distal femur revisited. Clin Orthop Relat Res 347: 43-56.
- Shewring DJ, Meggitt BF (1992) Fractures of the distal femur treated with the AO dynamic condylar screw. J Bone Joint Surg Br 74: 122-125.
- Siliski JM, Mahring M, Hofer HP (1989) Supracondylar-intercondylar fractures of the femur. J Bone Joint Surg Am 71: 95-103.
- Apostolou CD, Papavasiliou AV, Aslam N (2005) Preliminary results and technical aspects following stabilisation of fractures around the knee with liss. Injury 36: 529-536.
- Kanabar P,Kumar V, Owen PJ, Rushton N (2007) Less invasive stabilisation system plating for distal femoral fractures. J Orthop Surg 15: 299-302.
- Schandelmaier P, Partenhemer A, Koanemann B (2001) Distal femoral fractures and LISS stabilisation. Injury 32: 55-63.
- Syed AA, Agarwal M, Giannoudis PV (2004) Distal femoral fractures: long-term outcome following stabilisation with the LISS. Injury.;35:599–607
- Chen F, Mont MA, Bachner RS (1994) Management of ipsilateral supracondylar femur fractures following total knee arthroplasty. J Arthroplasty 9: 521-526.
- Figgie MP, Goldberg VM, Figgie HE, Sobel M (1990) The results of treatment of supracondylar fracture above total knee arthroplasty. J Arthroplasty 5: 267-276.
- Kobbe P, Klemm R, Reilmann H, Hockertz T.J (2008) Less invasive stabilisation system (LISS) for the treatment of periprosthetic femoral fractures: a 3-year follow-up. Injury 39: 472-479.
- Mize RD, Bucholz RW, Grogan DP (1982) Surgical treatment of displaced, communited fractured of the distal end of the femur. J Bone Joint Surg 64: 871-878.
- Fankhauser F, Gruber G, Schippinger G (2004) Minimal-invasive treatment of distal femoral fractures with the LISS (less invasive stabilization system). Acta Orthop Scand 75: 56-60.
- Frigg R, Appenzeller A, Christensen R (2001) The development of the distal femur less invasive stabilization system (LISS). Injury 32: 24-31.
- Muller ME, Allgower M, Schneider R, Willenegger H (1990) Manual of Internal fixation. Techniques reommended by the AOASIF Group. Springer-Verlag, NY, USA.
- Schütz M, Müller M, Krettek C (2001) Minimally invasive fracture stabilization of distal femoral fractures with the LISS: a prospective multicenter study. Results of a clinical study with special emphasis on difficult cases. Injury 32: 48-54
- Althausen PL, Lee MA, Finkemeier CG (2003) Operative stabilisation of supracondylar femur fractures above total knee arthroplasty: a comparison of four treatment methods. J Arthroplasty 18 :834-839.
- Borrelli J, Prickett W, Song E (2002) Extra osseous blood supply of the tibia and the effects of different plating techniques: a human cadaver study. J Orthop Trauma 16: 691.
- Farouk O, Krettek C, Miclau T (1997) Minimally invasive plate osteosynthesis and vascularity: preliminary results of a cadaver injection study. Injury 28: 7-13.
- Kumar V, Kanabar P, Owen P.J, Rushton N (2008) Less invasive stabilization system for the management of periprosthetic femoral fractures around hip arthroplasty. J Arthroplasty 23: 446-450
- Marti A, Fankhauser C, Frenk A (2001) Biomechanical evaluation of the less invasive stabilization system for the internal fixation of distal femur fractures. J Orthop Trauma 15: 482.
- Toole O, Gobezie RV, Hwang R (2006) Low complication rate of LISS for femur fractures adjacent to stable hip or knee arthroplasty. Clin Orthop Relat Res 450: 203-210.
- Perren SM (2002) Evolution of the internal fixation of long bone fractures. The scientific basis of biological internal fixation: choosing a new balance between stability and biology. J Bone Joint Surg 84: 1093-1110.
- Wick M, Muller EJ, Kutscha-Lissberg F (2004) Periprosthetic supracondylar femoral fractures: LISS or retrograde intramedullary nailing? Problems with the use of minimally invasive techniques. Unfallchirurg 107: 181-188.
- Miclau T, Holmes W, Martin RE, Krettek C, Schandelmaier P (1998) Plate osteosynthesis of the distal femur: surgical techniques and results. J South Orthop Assoc 7: 161-170.
- Yadav SS (1990) Dual-fibular grafting for massive bone gaps in the lower extremity. J Bone Joint Surg Am 72: 486-494.
- Mooney V, Nickel VL, Harvey JP Jr, Snelson R (1970) Cast-brace treatment for fractures of the distal part of the femur. A prospective controlled study of one hundred and fifty patients. J Bone Joint Surg Am 52: 1563-1578.
- Ostrum RF, Geel C (1995) Indirect reduction and internal fixation of supracondylar femur fractures without bone graft. J Orthop Trauma 9: 278-84
- Yang R, Liu H, Lui T (1990) Supracondylar fractures of the femur. J Trauma 30: 315-319.
- Wilson JN (1982) Watson Jone’s: Fractures and joint injuries. JAMA 6: 1003-1070.
- Chamley John (1951) The closed treatment of common fractures. JBJS 3: 197-198.
- Bank HH (1965) Healing of intraarticular fractures. Clin Orthop 40: 17-29.
- Neer CS, Gratham SA, Shelton ML (1967) Supracondylar fractures of adult femur. JBJS 49: 591-613.
- Mooney V, Nicke VL, Harvey JR (1970) Cast-brace treatment for fractures of the distal part of the femur. J Bone Joint Surg Am 52: 1563-1578.
- Connolly JF, Dehne E, Lafollette B (1973) Closed reduction and early cast-brace ambulation in the treatment of femoral fractures. J Bone Joint Surg Am 55: 1581-1599.
- Olerud S (1972) Operative treatment of supracondylar fractures of femur-Technique and results in 15 cases. JBJS 54: 1014-10032.
- Austin B, D’Arcy JC (1970) Internal fixation for supracondylar fracture of femur in elderly patients. JBJS 53: 420-24.
- Riggins RS, Garrick JG, Lipscomb PR (1972) Supracondylar fractures of femur-Survey of treatment. Clin Orthop 2:32-36.
- Pavel A, Smith RL (1974) Prophylactic antibiotic in clean orthopaedic surgery. JBJS 56: 777-782.
- Schatzker J, Lambert DC (1979) Supracondylar fractures of femur. Clin Orthop 138: 77-93.
- Zimmermann AJ (1979) Intraarticular fractures of distal femur. OCNA 10: 75-80.
- Donald SK, Bruckmann FR (1982) Rush pin fixation of supracondylar and intercondylar fractures of the femur. JBJS 64: 161-169.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences