Stab Wound In The Craniovertebral Spine: Case Report And Literature Review
Mamer S. Rosario, Mary Ruth A. Padua and Vernade May N. Santiago
Mamer S. Rosario*, Mary Ruth A. Padua and Vernadel May N. Santiago
Department of Orthopaedics, East Avenue Medical Center
- *Corresponding Author:
- Mamer S. Rosario
Medical Specialist Department of Orthopaedics
East Avenue Medical Center, EastAvenue
Diliman Quezon City Metro, Manila1101, Philippines
Tel: +639236863484
E-mail: vivek03sharma@rediffmail.com
Received date: October 24, 2015, Accepted date: November 07, 2015, Published date: November 14, 2015
Abstract
Study Design Case report and literature review.
Objective
To report the case of a patient who sustained a penetrating wound with a knife tip lodged in the craniovertebral spine and to review the literature.
Summary of Background Data
The incidence of vertebral artery injury (VAI) in penetrating neck trauma is around 7.4% for stab wounds. The surgical timing, approach and technique of foreign body removal are still controversial.
Methods
A 24-year-old male with a stab wound in the right occipital condyle presented with no neurologic deficits. Radiographs demonstrated a foreign body at the craniovertebral level. A CT angiogram was requested to rule out possible vertebral artery injury because of the level of injury. The knife tip was exposed using a posterior midline approach extended laterally to expose the occipital condyle, atlantal arch and vertebral artery. The knife was safely removed by being pulled along the axis of the knife trajectory.
Results
The patient had no complications during and after the operation.
Conclusion
Cases of spinal cord injury or vertebral artery injury in which the foreign body is retained are uncommonly reported. Computed tomography (CT) angiography is strongly suggested for cervical penetrating wounds to rule out vertebral artery injury. Surgical approach should be individualized to prevent any further injury to the cord, nerve roots and vertebral artery.
Keywords
Stab wound; Spinal cord injury; Vertebral artery injury; CT angiography
Introduction
Spinal cord injuries (SCIs) due to stab injuries are relatively rare (< 1.5% of SCIs) [1], and their surgical management is controversial [1-3]. The incidence of vertebral artery injury in penetrating neck trauma is around 7.4% for stab wounds [4]. We report a unique case of upper cervical spine impalement in which the knife tip was lodged in the occipitocervical level and our surgical strategy for foreign body removal.
Case Presentation
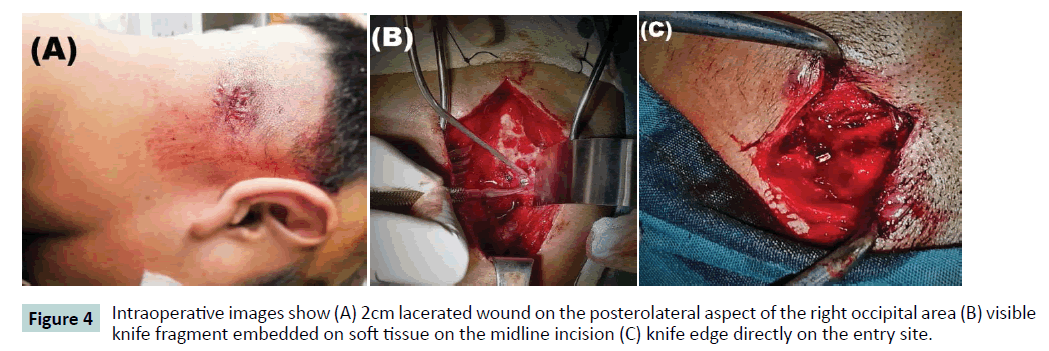
A 24 year-old bystander sustained a 2-cm stab wound to the right occipital condyle (Figure 4A). In the emergency department, the patient was fully conscious with no systemic signs or neurologic deficits.
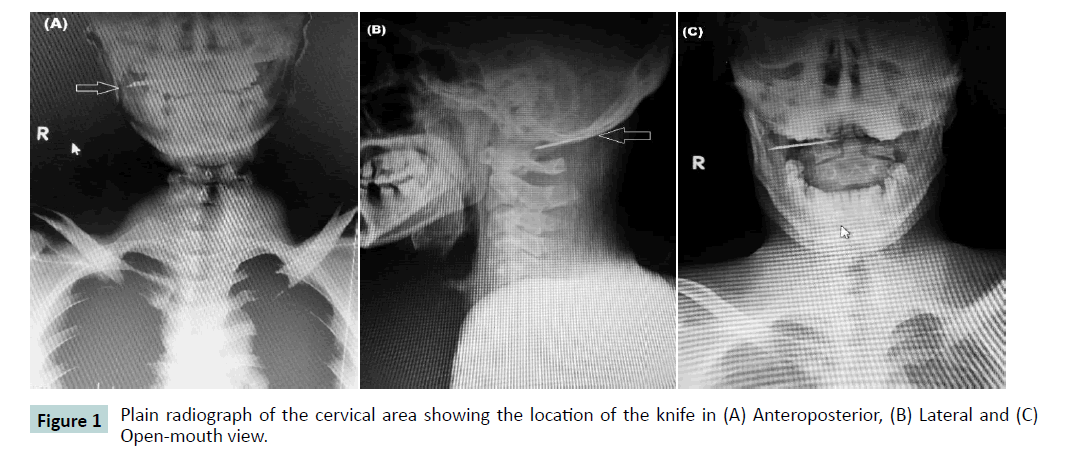
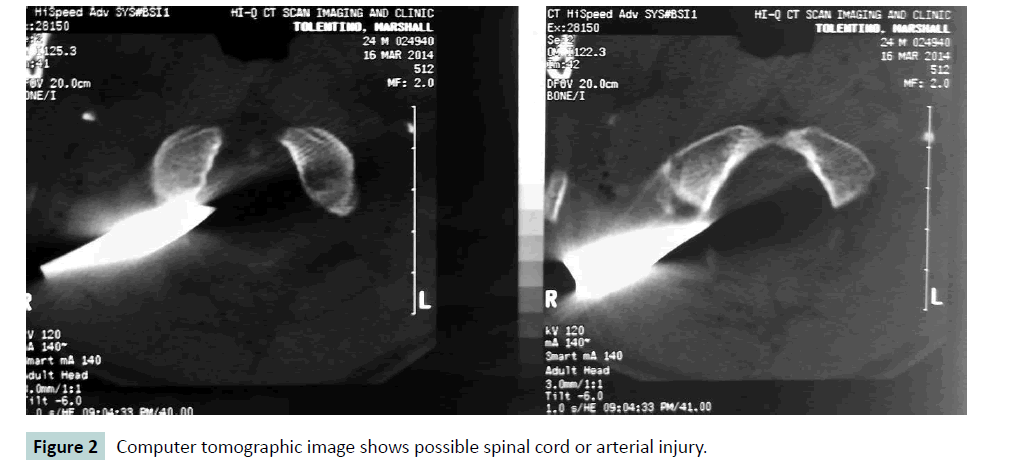
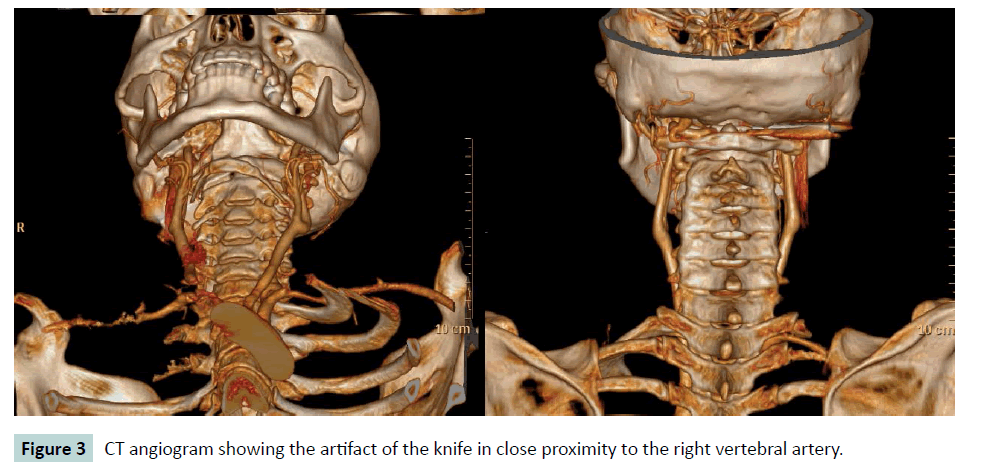
Plain cervical radiographs showed a retained foreign body that appeared to be part of a knife, but no obvious bony fracture was seen (Figure 1). A cervical computer tomographic (CT) scan revealed that the knife tip was lodged at the posterolateral aspect of the right occipital condyle. The images further revealed that the knife tip was located at the posterior rim of the atlantal arch at the level of the vertebral artery groove (Figure 2). CT-angiography was done preoperatively, documenting the close proximity of the knife tip to the vertebral artery as it emerges from the foramen transversarium of the atlas (Figure 3).
The patient was positioned prone, with the head secured using a Mayfield holder. A posterior midline incision was extended unilaterally at the level of the impalement. The goal was to visualize the occipital condyle, and the posterior arch of the atlas as landmarks. The vertebral artery at this level was carefully exposed. Intraoperatively, the tip of the foreign body was seen cephalad to the vertebral artery, and C1 nerve root (Figure 4B).
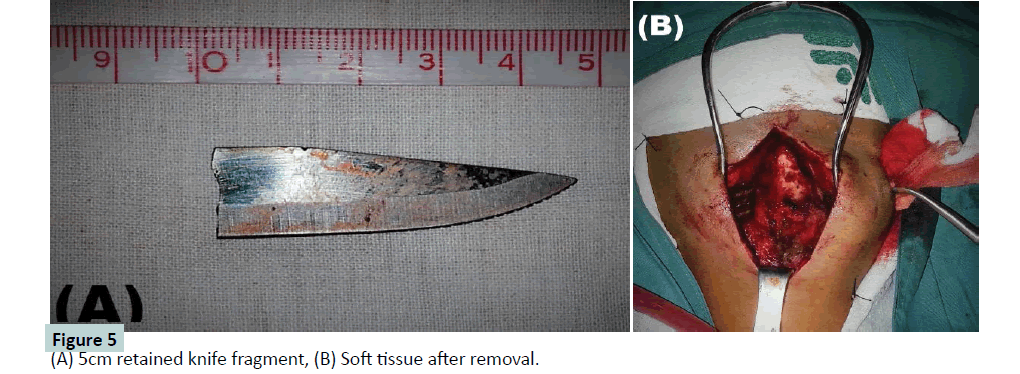
The knife tip was constantly visualized in relation to the vertebral artery while the assist dissected the entry wound and its track to expose the proximal end of the foreign body (Figure 4C). The spinal cord was protected by keeping the knife tip away from dura. Any rotational movement of the knife was avoided to prevent any injury to the nerve root and vertebral artery. The proximal end of the knife was secured and pulled longitudinally along the axis of the tract. The foreign body was a sharp knife that broke off from its handle (Figure 5A). After the foreign body was removed, debridement of devitalized tissues and copious irrigation of the wounds with saline solution was done (Figure 5B), and all wounds were primarily closed. Postoperative radiograph showed complete removal of foreign body with no visible bony fractures. Intravenous Cefazolin was given for seven days, and the patient was discharged ambulatory thereafter, with no neurologic deficits and no signs of infection.
Discussion
With stab wounds at the craniocervical junction, the knife blade is typically deflected by the occipital bone after traversing the subcutaneous tissue [5]. It slides on the undersurface of the occiput and is directed to the occiput-C2 space. However, damage to the vertebral artery or vein can be caused if the blade strikes the occiput-C1 articular mass [5].
Accurate imaging studies were essential in determining the exact location of the knife and in assessing for vertebral artery damage. Standard x-ray film and CT scan were necessary in simultaneously delineating the bony anatomy and trajectory of the knife [6]. The knife tip was shown penetrating the occiput-C1 articular mass, which alarmed the possibility of VAI in our case. A magnetic resonance imaging could not be performed due to ferromagnetic properties of the foreign body. As VAI was suspected, CT angiography was ordered preoperatively. Although catheter angiography has always been the “gold standard” for VAI diagnosis especially when the foreign body is near vital structures [7], a study by Inaba et al. [8] documented CT angiography to be 100% sensitive and 97.5% specific in detecting all clinically significant VAIs among all the penetrating neck injuries in the study.
It is recommended that sharp fragments (e.g., a knife tip) are removed irrespective of spinal level to prevent worsening of soft tissue or bony damage [9,10]. We also considered removing the foreign object to prevent the possible complication of leptomeningitis as reported by Gandhi et al. [11] in a cervical stab wound case, as well as delayed neurologic deficits [12] and intra spinal suppuration [13]. A posterior approach to the occipitocervical junction was carried out. As suggested by Horowitz et al. [14], extensive exposure is mandatory to permit extraction of the impaled object under direct vision. We did a posterior midline incision and exposed the posterior elements of the spine at the level of the impalement, with adequate extension enough to allow visualization of the vertebral artery and its spatial relationship to the knife tip. We avoided exposing the latter through the entry wound to prevent pushing motion of the knife tip that can nick the vertebral artery. The knife was pulled with the surgeon sure that the vertebral artery was not nicked.
Conclusion
Cervical spine stab wound with VAI and foreign body retention is uncommon, and appropriate examinations are necessary before a surgical removal is carried out. A suitable strategy should be chosen with the goal of safely removing the foreign object without causing iatrogenic cord, root, or arterial injury. CT angiography should be considered when VAI is suspected.
Key Points
1. Cervical stab wounds with spinal cord and/or vertebral artery injuries are relatively uncommon, especially those in which a foreign body is retained.
2. CT angiography is strongly suggested to ensure no penetrating neck injuries to the vertebral artery have occurred.
3. Surgical intervention in these cases remains controversial. However, the purpose of any surgery is to prevent infection, injury to the dura or vertebral artery that may cause CSF leakage or bleeding.
4. The surgical strategy is to ensure adequate exposure of the knife tip prior to removal to prevent any iatrogenic or further injury to the cord, vertebral artery, and nerve root.
References
- Hindman BJ, Palecek JP, Posner KL, et al. (2011) Cervical spinal cord, root, and bony spine injuries: a closed claims analysis. Anesthesiology 114:782-95.
- O’Neill S, McKinstry CS, Maguire SM. (2004)Unusual stab injury of the spinal cord. Spinal Cord 42:429-430.
- Seo BR, Lee JK, Lee JH, et al. (2009)An unusual stab wound causing a traumatic pseudomeningocele at the craniocervical junction. J ClinNeurosci 16:1365-1367.
- Karadag O, Gurelik M, Berkan O, et al. (2004) Stab wound of the cervical spinal cord and ipsilateral vertebral artery injury. Br J Neurosurg 18:545-547.
- Xia X, Zhang F, Lu F. (2012) Stab wound with lodged knife tip causing spinal cord and vertebral artery injuries. Spine 37:931-934.
- Jallo GI.( 1997) Neurosurgical management of penetrating spinal injury. SurgNeurol47:328-330.
- Gracias VH, Reilly PM, Philpott J, et al. (2001) Computed tomography in the evaluation of penetrating neck trauma. Arch Surg 136:1231-1235.
- Inaba K, Branco B, Menaker J et al. (2012) Evaluation of multidetector computed tomography for penetrating neck injury: a prospective multicenter study. J Trauma 72:576-584.
- Williams DT, Chang DL, DeClerck MP (2009) Penetrat ing spinal cord injuries with retained canal fragments. CJEM11:172-173.
- Manzone P, Domenech V, Forlino D (2001) Stab injury of the spinal cord surgically treated. J Spinal Disord14:264-267.
- Gandhi A, Saleem A, Sperling D et al.(2010) Leptomeningitis: a rare outcome after cervical stab wound. J Trauma68:57-60.
- Jones FD, Wooseley RE(1981) Delayed myelopathy secondary to retained intraspinal metallic fragment. Case report. J Neurosurg55:979-982.
- Kulkarni AV, Bhandari M, Stiver S, Reddy K (2000) Delayed presentation of spinal stab wound. Case report and review of literature. J Emerg Med 18:209-213.
- Horowitz MD, Dove DB, Eismont FJ, Green BA.( 1985) Impalement injuries. J Trauma 25: 914-916.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences