The Extent To Which Three Different Pain Measures Represent The Pain Experience Of People With Knee Osteoarthritis
Ahmed Negm, Joy c. MacDermid, Paul W. Stratford, Mohit Bhandari, Mitch Winemaker, Justin de Beer, Norma MacIntyre
Ahmed Negm1, Joy C. MacDermid1, Paul W. Stratford1, Mohit Bhandari2,3, Mitch Winemaker2,4, Justin de Beer2,4 and Norma MacIntyre1
1School of Rehabilitation Sciences, Mc-Master University, Hamilton, Ontario, Canada
2Division of Orthopaedics, Department of Surgery, Hamilton Health Sciences, Hamilton, Ontario, Canada
3Department of Clinical Epidemiology and Biostatistics, McMaster University, Hamilton, Ontario, Canada
4Hamilton Arthroplasty Group; Hamilton Health Sciences Juravinski Hospital, Hamilton, Ontario, Canada
- *Corresponding Author:
- Ahmed Negm
School of Rehabilitation Sciences, IAHS 403
McMaster University, 1400 Main St. W., Hamilton
Ontario, L8S 1C7, Canada
Tel: 905-525-9140 x21166
E-mail: negmam@mcmaster.ca
Abstract
Introduction Knee OA is the leading cause of pain and disability and half of people with knee OA experience significant pain that hinders daily activities. In the assessment of knee OA pain, the current focus is on pain intensity and associated disability, suggesting that the assessment of one dimension will reflect the other dimensions of chronic knee OA pain adequately. However, current studies dispute this assumption by showing fair correlation between scores on unidimensional disease-specific pain questionnaires and multidimensional ones. Appropriate pain measurement is critical to guide clinical decision-making. However, it�s been reported that no attempt has been made to ask patients with pain about whether current outcome measures are meaningful or whether the instructions, anchors or items included in the scales are capturing their pain experience adequately. The objective of this study is to determine if people with knee osteoarthritis (OA) prefer one of three self-report pain measures addressing different pain dimensions to represent their pain experience. Secondary objectives were to examine the correlation among measures and burden of completing these measures. Method Participants attending an orthopaedic outpatient clinic aged 40 y or older having idiopathic knee OA pain, minimal pain in other body parts, fluent in English, and cognitively competent were recruited for our cross sectional study. All consenting participants completed a demographic form and three pain measures were administered in a pre-determined order. The pain measures included 1) a generic, 11-point, single-item measure (Verbal Numeric Rating Scale, VNRS, maximum score = 10) asking about average pain intensity in the study knee in the past 24 hours; 2) a disease-specific, multi-item questionnaire (Intermittent and Constant Osteoarthritis Pain Questionnaire, ICOAP, maximum score = 44) asking about intensity and consistency of pain in the study knee over the past week; and 3) a generic, multi-item questionnaire (Short-Form McGill Pain Questionnaire-2, SF-MPQ-2, maximum score = 10) asking about somatic and affective dimensions of pain in the study knee over the past week. Higher scores indicate worse pain for all measures. After completing each measure, participants were asked how the measures fit their pain experience (FIT) by rating how well the pain measure described their experience of pain by placing a horizontal mark on a 10 cm FIT visual analogue scale where 0 = �Does not describe my pain at all� and 100 = �Describes my pain completely�. FIT scores for the three measures were compared using Freidman�s nonparametric repeated measures analysis of variance test. Associations between raw scores on the three pain measures were tested using Spearman rho correlation (rs). Findings 96 participants (57 females) had a mean (SD) age of 63.8(9.4) yr. The median of FIT score for the VNRS, ICOAP and SF-MPQ-2 was 7.5, 7.4, and 7.8cm, respectively, and did not differ (Ï?2 (2, N = 96) = 1.288, P = 0.5). The included participants had moderate knee OA pain intensity (median (IQR) score =6(5), 23(14.5), 2.4(3) for VNRS, ICOAP and SF-MPQ-2). Scores on the three measures were similarly associated (VNRS and ICOAP: rs=0.73(0.62, 0.81); VNRS and SF-MPQ-2: rs=0.69(0.56, 0.78); ICOAP and SF-MPQ-2: rs=0.70(0.58, 0.79). Conclusion: All three pain measures describe knee OA pain experience to a similar degree and scores were only moderately correlated. Differences in the pain attributes assessed may explain the finding that no one measure represented the experience of knee OA pain better than the other measures in our study sample.
Keywords
Chronic Pain; Pain Measurement; Patient Preference; Self-Report; Questionnaire; Scales
Introduction
Osteoarthritis (OA) is a very common chronic disease characterized by progressive symptoms and structural changes in the joint including articular cartilage loss, osteophytes, synovial inflammation and subchondral bone changes [1-3]. Almost half of the people diagnosed with OA experience significant pain and physical limitations during daily activities [4]. The knee is the most commonly affected joint and knee OA is the leading cause of pain and disability among older adults around the world [5,6]. Theoretically, pain has sensory, cognitive, and affective dimensions and each dimension requires measurement in order to acquire a comprehensive evaluation of the pain experience of people with chronic pain [7]. In the assessment of knee OA pain, the current focus is on pain intensity and associated disability, suggesting that the assessment of one dimension will reflect the other dimensions of chronic knee OA pain adequately. However, current studies dispute this assumption by showing fair correlations between scores on unidimensional disease-specific pain questionnaires and multidimensional ones [8,9].
The Verbal Numeric Rating Scale (VNRS) for pain intensity is a unidimensional measure that commonly used in knee OA research and clinical practice [10]. Knee OA pain typically is exacerbated by certain activities such as rising from chair, walking or climbing stairs [11]. Therefore, pain levels may be underestimated in people with knee OA if the measure does not assess pain during activity. Hence, disease-specific pain measures asking about pain during daily activities may be appropriate for people with knee OA [11]. The Intermittent and Constant Osteoarthritis Pain (ICOAP) questionnaire is a disease-specific 11-item measure [12]. The ICOAP was developed recently based on data from focus groups composed of people with hip and knee OA and asks about constant pain (five questions) and intermittent pain (six questions) [12]. Since consistency of knee OA pain predicts the need for total knee arthroplasty more strongly than pain intensity [13], the utility of measures addressing pain consistency needs to be explored. The revised version of the Short Form McGill Pain Questionnaire (SF-MPQ-2) is a multidimensional pain measure that addresses sensory (continuous, intermittent, neuropathic) and affective dimensions [14]. Since pain is a multidimensional construct [7], it may be that a multidimensional pain measure such as SF-MPQ-2 is more representative of the knee OA pain experience than a single-item unidimensional measure (VNRS) or a multi-item unidimensional disease-specific measure (ICOAP) addressing only the sensory dimension of pain in people with knee OA.
Pain is the main criterion for the clinical diagnosis of knee OA [15]. However, a gold standard for pain assessment in individuals with knee OA is not established and a combination of pain outcome measures is used in research and clinical practice [16]. Studies exploring the view of individuals with knee OA about pain measures are lacking. In 2010, an expert advisory group, the Initiative on Methods, Measurement and Pain Assessment in Clinical Trials (IMMPACT), reported that no attempt has been made to ask patients with pain about whether current outcome measures are meaningful or whether the instructions, anchors or items included in the scales are capturing their pain experience adequately [17]. More information is needed about the pain experience of people with knee OA and their views regarding the pain measures currently in use as this may help determine the most appropriate method(s) for assessing and treating pain in this population.
The primary objective of this study was to determine how well the pain experience of people with knee OA is represented by three self-report pain measures: VNRS, ICOAP, and SF-MPQ-2. Secondary objectives were to examine the burden of completing and scoring these three pain measures and the correlations between the scores and the global rating of knee OA severity provided by the physician.
Methods
Study Design
This study was a cross sectional Latin square design with participants completing all measures on one occasion in a predetermined order to balance any carryover effects [18]. Table 1 shows the order of administration of the pain measures for the first three participants. This order was repeated for all participants in the study. The study protocol was approved by Hamilton Health Science/McMaster Research Ethics Board and all participants provided written informed consent prior to any data collection.
| Order of Participant | Order of administration of pain measures | ||
|---|---|---|---|
| Participant 1 | VNRS | SF-MPQ-2 | ICOAP |
| Participant 2 | SF-MPQ-2 | ICOAP | VNRS |
| Participant 3 | ICOAP | VNRS | SF-MPQ-2 |
Table 1: The order of administration of the Verbal Numeric Rating Scale (VNRS), Short Form of McGill Pain Questionnaire-version 2 (SF-MPQ-2) and the Intermittent and Constant Osteoarthritis Pain Questionnaire (ICOAP) for the first three participants.
Participants
Study participants were men and women over the age of 40 years with clinical and radiological idiopathic knee OA according to the American College of Rheumatology modified clinical classification system [15] attending one of two orthopaedic surgery outpatient clinics affiliated with Hamilton Health Sciences and McMaster University. Eligible participants had knee pain and minimal pain in other joints or body parts. If the participant had bilateral knee pain, the study knee was decided to be the more symptomatic and if the same amount of pain was present in each knee, the study knee was to be selected by flipping a coin. Potential participants were excluded if they are unable to read, write or understand English or had any cognitive deficit resulting in an inability to provide informed consent or comprehend and comply with instructions.
Recruitment
Recruitment occurred between January 24 and April 12, 2013. Potential participants scheduled to attend for a regular clinic visit during this recruitment period were identified based on chart review and mailed an invitation letter. Those interested were telephoned to have questions answered, confirm eligibility, and schedule a single office visit.
Measures
The participants’ demographics including gender, age, ethnicity, level of education, height, weight, knee pain duration, pain medication use and the side of the painful (study) knee were collected. The participants completed three pain measures (described below). Upon completion of each pain measure, the participants were asked to rate how well each pain measure fit their pain experience (FIT score) by placing a vertical mark on a horizontal line 10 cm in length anchored at the left end by “= does not describe my pain at all” and at the right end by “= describes my pain completely”.
Pain Verbal Numeric Rating Scale
Participants were asked to verbally rate their pain level on a numeric scale from 0 (no pain) to 10 (worst pain imaginable), considering the amount of pain in the study knee that they have experienced on average over the past 24 hours. The VNRS has acceptable test–retest reliability in the knee OA population (ICC = 0.74) [19].
Intermittent and Constant Osteoarthritis Pain Questionnaire
Participants were asked to rate each of the 11 items on the ICOAP on a Likert scale from 0 (no pain) to 4 (worst pain) to describe pain over the past week [12]. A separate score was produced by summing the items for each of the two subscales (constant pain over the past week (5 items) and intermittent pain over the past week (6 items)) and a total score was calculated by summing the scores on the two subscales. The ICOAP has a high internal consistency (Cronbach’s alpha = 0.93), test-retest reliability (ICC = 0.85) and construct validity with Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) pain subscale (r = 0.81) in people with hip and knee OA [12].
Short form McGill Pain Questionnaire-version 2
On the SF-MPQ-2, participants were asked to describe pain symptoms over the past week addressing four subscales (constant pain (6 items), intermittent pain (6 items), neuropathic pain (6 items) and affective descriptors (4 items)) [14]. The response to each item was scored on an 11-point numeric rating scale (0 = none; 10 = worst possible). A total score was calculated by summing the scores for each items divided by the number of items. The SF-MPQ-2 has a high internal consistency (Cronbach’s alpha = 0.96) and construct validity (r = 0.72) with the Multidimensional Pain Inventory (MPI) severity scale in people with different pain condition (53% with various types of arthritis) [20].
Burden of completing and scoring the pain measures
Burden for respondents and administration was determined for each pain measure by recording the time (in seconds) taken to complete and score each pain measure and the number of errors made and questions asked during completion of each measure.
Physician global rating of knee OA severity
The attending surgeon provided a global rating of knee OA severity (PGROAS) for each patient on a 5-point Likert scale (0 = no OA and 4 = extremely severe) according to all the information available on the day of participant’s visit including the history, physical examination, and radiological assessment. The two surgeons were blinded to the patients' responses to the three pain questionnaires used for this study.
Data Analysis
SPSS 20 was used for the data analysis. Descriptive statistics were calculated to determine central tendencies and scores’ distributions. The normality was examined using the Shapiro-Wilk test. FIT scores for the three pain measures and time to complete and score the measures were not normally distributed. Therefore, we used the Freidman’s nonparametric analysis of variance test with the Freidman’s pairwise post hoc test to determine the effect of pain measures. Statistical significance was set a p < 0.05.
Based on the scores’ distributions, Pearson’s or Spearman’s correlations were used to examine the pairwise associations between scores on the three pain measures. Associations between PGROAS and the scores of all pain measures were estimated to know how well the self-reported pain scores correlate with the physician’s global rating. We were not able to calculate the sample size needed for this study due to the lack of any study with similar methodology in the literature.
Results
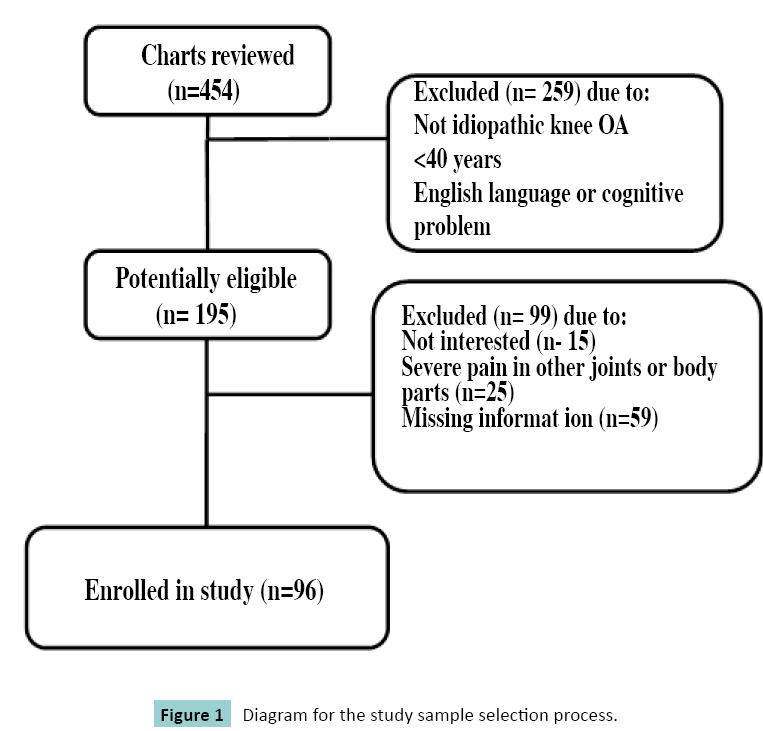
Figure 1 shows the flow through the study for all 454 patients screened and the reasons for exclusion of 99 patients deemed potentially eligible on chart review, resulting in inclusion of 96 participants. Participants’ demographics are shown in Table 2. Most of the participants were female (n = 57). Forty participants had bilateral knee pain but all of them had one knee worse than the other and the more painful knee was considered the study knee when completing the pain measures as per the protocol. Most of the participants (n = 86) did not remember completing any pain measures before participating in the study; 10 participants completed the VNRS previously. The level of education completed was equally split between secondary school (n = 46) and postsecondary education (college: n = 32; university, graduate studies: n = 17). All but 6 participants were White/Caucasians. Of the 96 participants, 60 reported no comorbidities with knee OA, 20 reported one comorbidity and 16 reported two or more comorbidities. Pain medications were taken for 77 participants. The median score and interquartile range (IQR) for each of the three pain measures are summarized in Table 2. According to PGROAS, 13 were mild, 38 were moderate, 40 were severe, and 5 were extremely severe.
| Variables | Mean (SD) |
|---|---|
| Age (y) | 63.81 (9.42) |
| Height (cm) | 169.65 (12.54) |
| Weight (kg) | 86.64 (18.51) |
| Body mass index (kg/m2) | 30.2 (5.9) |
| Knee pain duration (y) | 8.66 (9.33) |
| VNRS | *6 (5) |
| ICOAP | *23 (14.5) |
| SF-MPQ-2 | *2.4 (3) |
Table 2: Demographic characteristics and scores on pain measures for the 96 participants with knee osteoarthritis. *Data reported as Median (IQR) VNRS: Verbal Numeric Rating Scale (minimum 0, maximum10= worst pain); ICOAP: Intermittent and Constant Osteoarthritis Pain (minimum 0, maximum 44 = worst pain); SF-MPQ-2: Short Form McGill Pain Questionnaire version 2 = (minimum 0, maximum 10 = worst pain)
Representation of pain experience
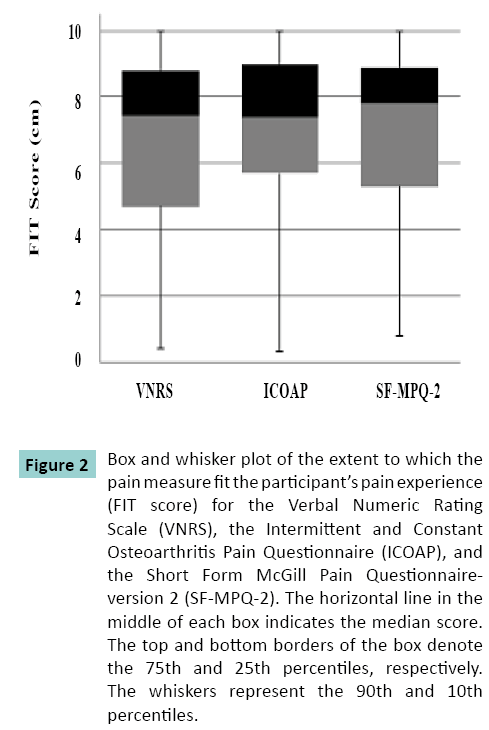
The median (IQR) FIT score was 7.5 (4), 7.4 (3.3) and 7.8 (3.6) cm, for VNRS, ICOAP and SF-MPQ-2 respectively. Figure 2 illustrates that no pain measure was more representative of the pain experience than the others (X2 = 1.288, df = 2, P = 0.50).
Figure 2: Box and whisker plot of the extent to which the pain measure fit the participant’s pain experience (FIT score) for the Verbal Numeric Rating Scale (VNRS), the Intermittent and Constant Osteoarthritis Pain Questionnaire (ICOAP), and the Short Form McGill Pain Questionnaireversion 2 (SF-MPQ-2). The horizontal line in the middle of each box indicates the median score. The top and bottom borders of the box denote the 75th and 25th percentiles, respectively. The whiskers represent the 90th and 10th percentiles.
Time to complete and score the pain measures
The median (IQR) time to complete the VNRS, ICOAP and SF-MPQ-2 was 20 (11.8), 126 (87.8), and 131(76.5) seconds, respectively and the main effect due to pain measure was significant (X2= 144.8, df= 2, P = 0.001). Post hoc tests showed that the VNRS was completed faster than both the ICOAP (P = 0.001) and SF-MPQ-2 (P = 0.001). There was no difference in the time taken to complete the ICOAP and SF-MPQ-2 (P = 0.36).
Median (IQR) time to score the VNRS, ICOAP and SF-MPQ-2 was 0 (0), 19 (17), and 37.5 (13.8) s, respectively and the main effect due to pain measure was significant (X2 = 190, df = 2, P = 0.001). Post hoc tests showed that the VNRS was scored faster than both the ICOAP (P = 0.001) and SF-MPQ-2 (P = 0.001). It took significantly less time to score the VNRS than either the ICOAP or the SF-MPQ and the ICOAP took less time to score than the SF-MPQ (P = 0.001).
Number of questions and errors
The total number of questions asked by the participants while completing the VNRS, ICOAP, and SF-MPQ-2 was 9 (asked by 9 participants), 21 (asked by 18 participants), and 57 (asked by 40 participants), respectively. The main effect due to pain measure was significant (X2 = 27.7, df = 2, P = 0.001) and post hoc tests confirmed that the participants asked more questions while completing the SF-MPQ-2 than while completing the VNRS (P = 0.001), or the ICOAP (P = 0.002). However, there was no significant difference between the number of question asked while completing the VNRS and the ICOAP (P= 0.50).
No errors were made when completing the VNRS and ICOAP whereas 24 errors were made when completing the SF-MPQ-2.
Correlations among the measures and PGROAS
Table 3 summarizes the associations between scores on the three pain measures and PGROAS.
| ICOAP | SF-MPQ-2 | PGROAS | |
|---|---|---|---|
| VNRS | 0.73 (0.62, 0.81) | 0.67 (0.56, 0.78) | 0.19 (-0.01, 0.38) |
| ICOAP | 0.70 (0.58, 0.79) | 0.07 (-0.14, 0.26) | |
| SF-MPQ-2 | 0.10 (-0.10, 0.29) |
Table 3: Spearman Correlation Coefficients (95% CI)) for associations between scores on the Verbal Numeric Rating Scale (VNRS), Intermittent and Constant Osteoarthritis Pain (ICOAP), Short Form McGill Pain Questionnaire-version 2 (SF-MPQ-2), and Physician Global Rating of Osteoarthritis Severity (PGROAS).
Discussion
In our sample of 96 people with knee OA recruited through orthopaedic surgeons’ clinics, their pain experience was represented similarly by a generic unidimensional single item pain measure (i.e., VNRS), a disease-specific unidimensional multiple item pain measure (i.e., ICOAP), and a generic multidimensional multiple item pain measure (i.e., SF-MPQ-2). The order in which the pain measures were completed was controlled using a Latin square design and the participants were immediately asked to record the degree to which the measure represented their pain experience thereby limiting the influence of factors such as fatigue, learning and recall. These results can be interpreted in two ways. Perhaps pain intensity, which is addressed in all three pain measures administered in our study, is an adequate indicator of the pain experience in people with knee OA pain. Alternatively, the additional participant burden associated with completing the ICOAP, evaluating a single dimension of pain using multiple disease-specific items, and the SF-MPQ-2, evaluating multiple dimensions of pain using multiple generic items, was offset by the fact that different information regarding the pain experience was conveyed which was valued by the participants. The moderate correlations between pain measure scores support the latter interpretation.
The median pain scores for our sample are comparable to scores on the same pain measures reported previously for OA population with similar characteristics. A mean VNRS score of 7 (versus a median score of 6 for our 96 participants) was reported for a sample of 347 participants attending a specialty rheumatology outpatient clinic for knee or hip OA problems comparable to our sample in age (mean (SD) = 55 (10) y), BMI (mean (SD) = 29 (5) kg/m2 ) and gender distribution (67% female) [21]. A similar ICOAP score (mean = 26) was reported for 109 individuals with knee OA attending physical therapy outpatient clinics who were comparable in age (mean (SD) 68 (8.4) y), BMI (mean (SD) 29.9 (4.5) kg/m2 ) and gender distribution (60.6% female). In contrast to our sample, most participants (63.3%) in the study by Goncalves et al (2012) had bilateral knee OA [22]. Our participants had a similar score on the SF-MPQ-2 as 71 people with knee and hip OA on the waiting list for primary hip or knee joint replacement surgery (mean SF-MPQ score = 2.7). Apart from the severity of knee OA, the waitlisted sample was similar to the participants in the current study with respect to age and gender distribution [23]. This finding increases the generalizability of our result. Our study shows that no one pain measure was more representative of the experience of knee OA pain than the other two. Participants completed the VNRS in the shortest time and scoring took the least amount of time. Moreover, the participants asked the least number of questions while completing the VNRS and no errors were encountered. For these reasons, we recommend using the VNRS to evaluate pain in people with knee OA in the clinical setting if time constraints preclude the use of more than one pain measure.
This is the first study to explore the extent to which pain measures capture the pain experience of people with knee OA specifically. Few studies address this topic in people with chronic pain. Peters et al (2007) examined patient preference for pain measures in terms of ease of understanding and completion [24]. Preference among five generic unidimensional single item measures of pain intensity (Horizontal VAS, Vertical VAS, Verbal Descriptor Scale, Box-11 Numeric Rating Scale (Box-11) and Box-21 Numeric Rating Scale (Box-21)) was evaluated in a group of people with chronic pain due to various musculoskeletal conditions who had characteristics similar to our participants with chronic knee OA pain (mean age of 54 years, 63% female, 52% completed elementary school) [24]. Almost half of the participants (49%) preferred the Box-21 [24]. In another study [25], participants with acute post-operative pain were asked to identify their preferred pain measure among five generic unidimensional single item pain measures (the Verbal Descriptor Scale, the Numeric Box- 11, the Faces Pain Scale, the Numeric Box-21 Scale, and the Colored Analogue Scale) and the effect of age on preference was examined [25]. The authors concluded that the Faces Pain Scale is the most preferred scale across the study sample (mean (SD) age = 55.6 (15.6) y), although, the young adults (20-44 y) preferred the Numeric Box-11 [25]. Due to the difference in methodology, sample population and the theoretical basis, our study results are not comparable directly.
In our study sample, scores on the VNRS, ICOAP and SF-MPQ-2 were moderately correlated. This finding suggests that the three measures are evaluating different pain attributes. Our findings are consistent with other studies reporting correlations between different pain measures (8, 12, 26). For example, Gandhi et al (2010) found the scores on the WOMAC pain subscale and SF-MPQ were moderately correlated (r = 0.36) (8). On the other hands, measures evaluating the same attribute are highly correlated. For example, Hawker et al (2008) concluded that scores on the ICOAP and WOMAC pain subscale were highly correlated among 82 people with knee OA (r = 0.81) [12] which may indicate that scores on multiple item disease-specific pain measures have higher associations. Similarly, the correlation between scores on two single item generic measures of pain intensity, such as the VNRS and VAS, is very high (r = 0.91) [26]. These observations confirm that the moderate correlations in our study may be explained by differences in the pain dimensions addressed.
In knee OA evaluation, surgeons usually focus on range of motion, alignment, and stability (not pain), but people with knee OA focus on the functionality of the knee as a whole (including pain) [27]. Therefore, the lack correlations between pain measure scores and PGROAS (r = 0.1) were expected. Bullins et al (2001) noted the disagreement between physicians and patients regarding evaluation of disease severity based on a poor correlation between an objective physician-assessed knee score and the patient-reported satisfaction score following total knee arthroplasty [27]. Another study involving a sample of people with knee OA similar to our study found no correlation between scores on the WOMAC pain subscale and the physician assessment of radiological knee OA based on Kellgren-Lawrence scale [28]. All the included participants in our study had radiological knee OA; therefore, the lack of correlation we observed may reflect the lower weight given to the patient’s reported pain level in determining knee OA severity than to the radiological and clinical findings from the physician’s perspective.
The results of our study must be considered in the context of the limitations. We recruited people with knee OA attending clinics of orthopaedic surgeons affiliated with a teaching hospital. The extent to which the findings can be generalized to other clinical settings is unknown. The participants in the study filled out the pain measures in an interview setting (one to one) with no time limit which does not reflect usual practice in this busy clinical setting and we are not sure if the findings related to burden (errors and questions) would differ if participants were asked to complete the measures independently. Only three pain measures were administrated in this study to decrease the burden on the participants; the inclusion of different pain measures may have yielded different results.
Conclusion
We asked people with knee OA pain, the most common cause of chronic musculoskeletal pain, to identify which of three pain measures best represented their pain experience. No pain measure was identified as more representative of their knee OA pain experience among the VNRS, the ICOAP or the SF-MPQ-2. The moderate associations between pain measure scores confirmed that the three measures assess different pain attributes, thus a combination of pain measures may best represent the pain experience of people with knee OA. In a clinical setting able to administer only one pain measure for to patients with knee OA, the VNRS is recommended since it is quick to complete and score.
Author contributions
All authors made substantial contributions to the conceptualization, design, data collection, analysis, interpretation, drafting and revisions; and approved the final version.
Conflict of interest
None of the authors has any financial and personal relationships with other people or organizations that could potentially and inappropriately influence this work and its conclusions.
References
- Bennell KL, Hunter DJ, Hinman RS (2012 ) Management of osteoarthritis of the knee BMJ. 30; 345: e4934.
- Jaiprakash A, Prasadam I, Feng JQ, Liu Y, Crawford R et al. (2012) Phenotypic characterization of osteoarthritic osteocytes from the sclerotic zones: A possible pathological role in subchondral bone sclerosis. Int J Biol Sci 8: 406-417.
- Troeberg L, Nagase H (2012) Proteases involved in cartilage matrix degradation in osteoarthritis Biochim Biophys Acta 1824: 133-145.
- Centers for Disease Control and Prevention (CDC) (2010) Prevalence of doctor-diagnosed arthritis and arthritis-attributable activity limitation - United States, 2007-2009. MMWR - Morbidity & Mortality Weekly Report 59: 1261-1265.
- Lawrence RC, Felson DT, Helmick CG, Arnold LM, Choi H, Deyo RA, et al. (2008) Estimates of the prevalence of arthritis and other rheumatic conditions in the united states. part II. Arthritis Rheum 58: 26-35.
- Quintana JM, Arostegui I, Escobar A, Azkarate J, Goenaga JI (2008) Prevalence of knee and hip osteoarthritis and the appropriateness of joint replacement in an older population. Arch Intern Med 168: 1576-1584.
- Melzack R (2004) Evolution of the neuromatrix theory of pain the prithvi raj lecture: Presented at the third world congress of world institute of pain, barcelona. Pain Pract : 85-94.
- Gandhi R, Tsvetkov D, Dhottar H, Davey JR, Mahomed NN (2010) Quantifying the pain experience in hip and knee osteoarthritis. Pain Res Manag 15: 224-228.
- Roth ML, Tripp DA, Harrison MH, Sullivan M, Carson P (2007) Demographic and psychosocial predictors of acute perioperative pain for total knee arthroplasty Pain Res Manag 12: 185-194.
- Dworkin RH, Peirce-Sandner S, Turk DC, McDermott MP, Gibofsky A, Simon LS, et al. (2011) Outcome measures in placebo-controlled trials of osteoarthritis: Responsiveness to treatment effects in the REPORT database. Osteoarthritis Cartilage 19: 483-492.
- Tsai PF, Tak S (2003) Disease specific pain measures for osteoarthritis of the knee or hip. Geriatr Nurs. 24:106-109.
- Hawker GA, Davis AM, French MR, Cibere J, Jordan JM, March L, et al. (2008) Development and preliminary psychometric testing of a new OA pain measure-an OARSI/OMERACT initiative. Osteoarthritis Cartilage 16: 409-414.
- Wise BL, Felson DT, Clancy M, Niu J, Neogi T, Lane NE, et al. (2011) Consistency of knee pain and risk of knee replacement: The multicenter osteoarthritis study. J Rheumatol. 38: 1390-1395.
- Dworkin RH, Turk DC, Revicki DA, Harding G, Coyne KS, Peirce-Sandner S, et al. (2009) Development and initial validation of an expanded and revised version of the short form McGill pain questionnaire (SF-MPQ-2). Pain. 144:35-42.
- Altman R, Asch E, Bloch D, Bole G, Borenstein D, Brandt K, et al. (1986) Development of criteria for the classification and reporting of osteoarthritis. classification of osteoarthritis of the knee. Diagnostic and therapeutic criteria committee of the American Rheumatism Association. Arthritis & Rheum.29: 1039-49.
- Bartlett SJ, Ling SM, Mayo N, Scott S, Bingham III CO (2011) Identifying common trajectories of joint space narrowing over two years in knee osteoarthritis. Arthritis Care Res. 63:1722-1728.
- Turk DC. Dworkin RH. Burke LB. Gershon R. Rothman M. Scott J. et al. (2006) Initiative on Methods,Measurement and Pain Assessment in Clinical Trials. Developing patient-reported outcome measures for pain clinical trials: IMMPACT recommendations. Pain.125: 208-215.
- Bradley JV. (1958) Complete counterbalancing of immediate sequential effects in a Latin square design. J Am Stat Assoc. 53: 525-528.
- Ruyssen-Witrand A, Fernandez-Lopez CJ, Gossec L, Anract P, Courpied JP et al. (2011) Psychometric properties of the OARSI/OMERACT osteoarthritis pain and functional impairment scales: ICOAP, KOOS-PS and HOOS-PS. Clin Exp Rheumatol.29: 231-237.
- Lovejoy TI, Turk DC, Morasco BJ. (2012) Evaluation of the psychometric properties of the revised short form McGill pain questionnaire. J Pain. 13: 1250-1257.
- Snijders GF, van den Ende CH, van den Bemt BJ, van Riel PL, van den Hoogen FH, den Broeder AA, et al. (2012) Treatment outcomes of a numeric rating scale (NRS)-guided pharmacological pain management strategy in symptomatic knee and hip osteoarthritis in daily clinical practice. Clin Exp Rheumatol. 30:164-170.
- Goncalves RS, Meireles AC, Gil JN, Cavalheiro LM, Rosado JO, Cabri J. (2012) Responsiveness of intermittent and constant osteoarthritis pain (ICOAP) after physical therapy for knee osteoarthritis. Osteoarthritis Cartilage.20:1116-1119.
- Grafton KV, Foster NE, Wright CC (2005) Test-retest reliability of the short form McGill pain questionnaire: Assessment of intraclass correlation coefficients and limits of agreement in patients with osteoarthritis. Clin J Pain. 21: 73-82.
- Peters ML, Patijn J, Lame I (2007) Pain assessment in younger and older pain patients: Psychometric properties and patient preference of five commonly used measures of pain intensity. Pain Medicine.8:601-610.
- Zhou Y, Petpichetchian W, Kitrungrote L (2011) Psychometric properties of pain intensity scales comparing among postoperative adult patients, elderly patients without and with mild cognitive impairment in China. Int J Nurs Stud. 48: 449-457.
- Downie WW, Leatham PA, Rhind VM, Wright V, Branco JA et al.(1978) Studies with pain rating scales. Ann Rheum Dis. 37: 378-381.
- Bullens PH, van Loon CJ, de Waal Malefijt MC, Laan RF, Veth RP (2001) Patient satisfaction after total knee arthroplasty: A comparison between subjective and objective outcome assessments. J Arthroplasty.16:740-747.
- Cubukcu D, Sarsan A, Alkan H (2012) Relationships between pain, function and radiographic findings in osteoarthritis of the knee: A cross-sectional study. Arthritis. 98: 40-60.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences